Wednesday, September 29, 2010
Arts at the Heart feature on Big Society
To read Clive Parkinson's paper on Big Society, go to: http://www.nalgao.org/e107_images/custom/aahseptfinal1b.pdf
Tuesday, September 28, 2010
Income, obesity, and heart disease in US states
The figure below combines data on median income by state (bottom-left and top-right), as well as a plot of heart disease death rates against percentage of population with body mass index (BMI) greater than 30 percent. The data are recent, and have been provided by CNN.com and creativeclass.com, respectively.
Heart disease deaths and obesity are strongly associated with each other, and both are inversely associated with median income. US states with lower median income tend to have generally higher rates of obesity and heart disease deaths.
The reasons are probably many, complex, and closely interconnected. Low income is usually associated with high rates of stress, depression, smoking, alcoholism, and poor nutrition. Compounding the problem, these are normally associated with consumption of cheap, addictive, highly refined foods.
Interestingly, this is primarily an urban phenomenon. If you were to use hunter-gatherers as your data sources, you would probably see the opposite relationship. For example, non-westernized hunter-gatherers have no income (at least not in the “normal” sense), but typically have a lower incidence of obesity and heart disease than mildly westernized ones. The latter have some income.
Tragically, the first few generations of fully westernized hunter-gatherers usually find themselves in the worst possible spot.
Heart disease deaths and obesity are strongly associated with each other, and both are inversely associated with median income. US states with lower median income tend to have generally higher rates of obesity and heart disease deaths.
The reasons are probably many, complex, and closely interconnected. Low income is usually associated with high rates of stress, depression, smoking, alcoholism, and poor nutrition. Compounding the problem, these are normally associated with consumption of cheap, addictive, highly refined foods.
Interestingly, this is primarily an urban phenomenon. If you were to use hunter-gatherers as your data sources, you would probably see the opposite relationship. For example, non-westernized hunter-gatherers have no income (at least not in the “normal” sense), but typically have a lower incidence of obesity and heart disease than mildly westernized ones. The latter have some income.
Tragically, the first few generations of fully westernized hunter-gatherers usually find themselves in the worst possible spot.
Monday, September 27, 2010
RAMBERT DANCE: AWAKENINGS
Much of the arts and health movement is concerned with the instrumental impact of the arts, with organisations like Arts for Health striving to engage marginalised communities in creative and cultural activity that might impact on well-being. There is ample evidence that illustrates engaging in the arts not only improves physical and mental health, but the very act of bringing people together provides something of the civic glue to healthy communities.
The implicit impact of the arts in relation to health and well-being however, is harder to define. Many interesting studies illustrate that the theatre and gallery-going public are more likely to be the educated middle-classes, and that people marginalised by issues such as mental ill-health are far less likely to participate in cultural opportunities because of broad ranging social and economic barriers.
For someone with limited experience of contemporary dance, an invitation to the Lowry to watch a new piece of dance being premiered could have made for a challenging evening. The Lowry was full to capacity for this premiere of Rambert Dance Company’s interpretation of the work of Dr Oliver Sacks, Awakenings, already made famous by the Hollywood film of the same name,
As its stimulus, Awakenings, uses the true story of a group of patients affected by sleeping sickness following the 1918 flu pandemic. Through the prescription of the drug L-Dopa, the patients who had been in a catatonic state for decades become suddenly animated, but the drug’s effects are short lived and this brief period of lucidity is marred by seizures and delirium, with patients ultimately slipping back into a twilight world.
This performance visually and physically captures the passage of treatment, from the liberation of symptoms to the subsequent relapse of the patients. For the audience and dancers, the music replaces the drug L-Dopa and offers us the opportunity to connect viscerally to the isolated and disjointed worlds of the individuals affected by this strange sleeping sickness.
The unpredictability of the tics and twitches of this condition were made manifest by the dancers as they entered, walking backwards onto the stage, as if wary and watchful of their condition. Suddenly, we would see their bodies contract in spasm, accompanied by spikes of music. In contrast were the darker moments, when a percussive thrum reflected the depressive slump of the patients; the dancer’s bodies heavy with the burden of this illness.
There was a real sense of tension in the audience, watching people dressed as if for work on a summer’s day on Madison Avenue, literally frozen in their tracks, as they made their way to or from their destination. We had the impression that they were locked into a world entirely within them-selves and that all they could do was to observe the effects of the condition as it took over them.
On the empty stage, the elegantly dressed and beautifully lithe performers made visible something of the internal landscape of the patients they inhabited. But what relevance to this arts and health agenda is there?
Having worked with a wide range of communities who believe that the ‘high-arts’ have nothing to do with them, I’m aware that dance or ballet is often dismissed as inaccessible to people who haven’t experienced it. I am often looking for ways to describe disease, illness or concepts of well-being and frequently words are insufficient. What I crave are universal metaphors that reach out beyond the confines of language or cultural experience and beyond the common assumptions that status is a barrier to appreciating subtle or complex ideas.
It would be easy to argue that Awakenings was very unambiguous and without a need for tricky interpretation or you may share my view, that this visceral manifestation of what it is to be human and to have free will, only for that free will be taken away, makes both fluid and solid the potential and frustration that our fleeting experience of life offers.
It would be easy to argue that Awakenings was very unambiguous and without a need for tricky interpretation or you may share my view, that this visceral manifestation of what it is to be human and to have free will, only for that free will be taken away, makes both fluid and solid the potential and frustration that our fleeting experience of life offers.
Twists Series: Maintenance II
"I have short hair (about 4 to 5inches) and whenever I twist my hair it twists up on itself so they look like they're sticking out all over my head. How do I get them to all lie straight down?"
I had a similar situation when I was at that stage. What helped was to twist my hair wet as opposed to dry. Doing that allowed for the water to weigh down the twists. Once the twists airdried, they would remain down with the help of wrapping with a scarf nightly. The longer your hair grows, the less they will stick out. When I hit about 8-9 inches, my twists no longer stuck out.
"How do you keep them moist?"
I spritz weekly with water until damp and then apply whipped shea butter. I also wear updos 95% of the time, which involves tucking the ends of my twists under.
"What do you do to the ends when they are dry or ragged looking (or is it just time for a trim!?)"
•When my ends are dry, I revive them with water and whipped shea butter. Sometimes, my dry ends call for a fresh wash.
••When they get ragged looking and even thin, I tend to trim them. Raggedness sometimes implies damaged ends. Additionally, such ends may cause damage to the healthy ones. Ragged, thin ends make it harder for me to undo my twists and easier for tangles and knots to form. Thus, I trim them away. In between trims, I try to minimize tasks that contribute to thin, ragged ends ... such as impatience during detangling and twist takedown, sleeping on cotton pillowcases without a protective barrier (e.g., satin scarf), etc.
"Is it more important to not touch the hair in the twists for say a week minimum or to keep it in a style that will retain moisture and protect the ends? I ask this since the front of my hair especially gets extremely fuzzy after 2 to 3 days of fresh twists!"
•In order to retain length, it is more important to wear styles that retain moisture and protect the ends than to not touch one's twists for a week. It is more important to pin up the twists daily and take it down nightly than to wear the pinned style 24-7 and risk hairline damage. It is more important to touch the hair with moisture and risk fuzz than to not touch the hair and risk dryness. In other words, properly caring for your twists may require some touching within the week, which is fine. Health supersedes no fuzz.
••For a future topic, I'll talk about how to twist such that fuzz is minimized.
••For a future topic, I'll talk about how to twist such that fuzz is minimized.
"Did you experience alot of matting and knotting when leaving the twists in for even short periods of time?"
Short answer: It depends. What I've learned is that I get the most matting and knotting when: 1) I wash more than twice during a twist period and 2) don't detangle thoroughly between twist sessions. Even if it's a short period in twists, matting and knotting will occur if I do #1 and/or #2. With my current regimen (twists for 3 weeks, 1-2x washes), I get no matting and very little knotting.
"I noticed some ppl do twists for say a week then use the twist out on the weekend...does this act as being counter - productive?"
I used this method during my in-between stage (between TWA and BAA) and it worked out well. It's ideal for those who like to wear their hair out but do not want to sacrifice the health and length retention. It is only counter-productive if one is pinched for time; such a method requires weekly detangling and re-twisting. Other than the time factor, it is a good method.
"Soul" Food Mondays || Increasing Patience
 |
| {Image Source} |
Patience is necessary to attain a healthy soul. It goes hand in hand with perseverance. With strength. With wisdom. With faith and hope. Patience keeps stress, anger, and anxiety at bay. It is always rewarded and brings peace of mind. Patience is what you'll find in the strongest and healthiest of relationships.
Increase your patience, and your soul will thank you for it.
"Learn the art of patience. Apply discipline to your thoughts when they become anxious over the outcome of a goal. Impatience breeds anxiety, fear, discouragement and failure. Patience creates confidence, decisiveness, and a rational outlook, which eventually leads to success." ~Brian Adams
"If you are patient in one moment of anger, you will escape a hundred days of sorrow." ~Chinese Proverb
"One minute of patience, ten years of peace." ~Greek proverb
"Our patience will achieve more than our force." ~Edmund Burke
Labels:
Soul,
Soul Food Mondays
Sunday, September 26, 2010
Training a new generation of clinicians
On Saturday September 25th, the Jefferson School of Population Health was the site of a unique training program designed to help create a new generation of clinicians fluent in the language of measuring and improving the quality and safety of healthcare. With support from Lilly, we hosted dozens of trainees from mutiple schools throughout the Northeast. They assembled to hear from faculty like David Mayer MD at the University of Illinois talk about creating a new culture of practice characterized by openess and patient centeredness. They got to hear David LindquistMD from Brown Medical School demonstrate the power of medical simulation training for safety and quality improvement. They also heard from Lia Logio MD from Cornell Medical College talk about creating a training environment that recognizes different cultures, and thereby improves the quality of care.Learners from all of these schools will themselves become leaders and they will spread this gospel to help change undergraduate medical education (UME) and graduate medical education (GME)in new and exciting ways. While the ACGME in Chicago is working to mandate new types of reporting, from resident involvment in medical error to measuring the outcomes of residency training, these new learners will be prepared to meet this challenge. What are your trainees doing to keep up with this critical national trend?? How can we prepare the next generation of clinicians in the disciplines of quality measurement and safety improvement?? DAVID NASH
Wednesday, September 22, 2010
Low nonexercise activity thermogenesis: Uncooperative genes or comfy furniture?
The degree of nonexercise activity thermogenesis (NEAT) seems to a major factor influencing the amount of fat gained or lost by an individual. It also seems to be strongly influenced by genetics, because NEAT is largely due to involuntary activities like fidgeting.
But why should this be?
The degree to which different individuals will develop diseases of civilization in response to consumption of refined carbohydrate-rich foods can also be seen as influenced by genetics. After all, there are many people who eat those foods and are thin and healthy, and that appears to be in part a family trait. But whether we consume those products or not is largely within our control.
So, it is quite possible that NEAT is influenced by genetics, but the fact that NEAT is low in so many people should be a red flag. In the same way that the fact that so many people who eat refined carbohydrate-rich foods are obese should be a red flag. Moreover, modern isolated hunter-gatherers tend to have low levels of body fat. Given the importance of NEAT for body fat regulation, it is not unreasonable to assume that NEAT is elevated in hunter-gatherers, compared to modern urbanites. Hunter-gatherers live more like our Paleolithic ancestors than modern urbanites.
True genetic diseases, caused by recent harmful mutations, are usually rare. If low NEAT were truly a genetic “disease”, those with low NEAT should be a small minority. That is not the case. It is more likely that the low NEAT that we see in modern urbanites is due to a maladaptation of our Stone Age body to modern life, in the same way that our Stone Age body is maladapted to the consumption of foods rich in refined grains and seeds.
What could have increased NEAT among our Paleolithic ancestors, and among modern isolated hunter-gatherers?
One thing that comes to mind is lack of comfortable furniture, particularly comfortable chairs (photo below from: prlog.org). It is quite possible that our Paleolithic ancestors invented some rudimentary forms of furniture, but they would have been much less comfortable than modern furniture used in most offices and homes. The padding of comfy office chairs is not very easy to replicate with stones, leaves, wood, or even animal hides. You need engineering to design it; you need industry to produce that kind of thing.
I have been doing a little experiment with myself, where I do things that force me to sit tall and stand while working in my office, instead of sitting back and “relaxing”. Things like putting a pillow on the chair so that I cannot rest my back on it, or placing my computer on an elevated surface so that I am forced to work while standing up. I tend to move a lot more when I do those things, and the movement is largely involuntary. These are small but constant movements, a bit like fidgeting. (It would be interesting to tape myself and actually quantify the amount of movement.)
It seems that one can induce an increase in NEAT, which is largely due to involuntary activities, by doing some voluntary things like placing a pillow on a chair or working while standing up.
Is it possible that the unnaturalness of comfy furniture, and particularly of comfy chairs, is contributing (together with other factors) to not only making us fat but also having low-back problems?
Both obesity and low-back problems are widespread among modern urbanites. Yet, from an evolutionary perspective, they should not be. They likely impaired survival success among our ancestors, and thus impaired their reproductive success. Evolution “gets angry” at these things; over time it wipes them out. In my reading of studies of hunter-gatherers, I don’t recall a single instance in which obesity and low-back problems were described as being widespread.
But why should this be?
The degree to which different individuals will develop diseases of civilization in response to consumption of refined carbohydrate-rich foods can also be seen as influenced by genetics. After all, there are many people who eat those foods and are thin and healthy, and that appears to be in part a family trait. But whether we consume those products or not is largely within our control.
So, it is quite possible that NEAT is influenced by genetics, but the fact that NEAT is low in so many people should be a red flag. In the same way that the fact that so many people who eat refined carbohydrate-rich foods are obese should be a red flag. Moreover, modern isolated hunter-gatherers tend to have low levels of body fat. Given the importance of NEAT for body fat regulation, it is not unreasonable to assume that NEAT is elevated in hunter-gatherers, compared to modern urbanites. Hunter-gatherers live more like our Paleolithic ancestors than modern urbanites.
True genetic diseases, caused by recent harmful mutations, are usually rare. If low NEAT were truly a genetic “disease”, those with low NEAT should be a small minority. That is not the case. It is more likely that the low NEAT that we see in modern urbanites is due to a maladaptation of our Stone Age body to modern life, in the same way that our Stone Age body is maladapted to the consumption of foods rich in refined grains and seeds.
What could have increased NEAT among our Paleolithic ancestors, and among modern isolated hunter-gatherers?
One thing that comes to mind is lack of comfortable furniture, particularly comfortable chairs (photo below from: prlog.org). It is quite possible that our Paleolithic ancestors invented some rudimentary forms of furniture, but they would have been much less comfortable than modern furniture used in most offices and homes. The padding of comfy office chairs is not very easy to replicate with stones, leaves, wood, or even animal hides. You need engineering to design it; you need industry to produce that kind of thing.
I have been doing a little experiment with myself, where I do things that force me to sit tall and stand while working in my office, instead of sitting back and “relaxing”. Things like putting a pillow on the chair so that I cannot rest my back on it, or placing my computer on an elevated surface so that I am forced to work while standing up. I tend to move a lot more when I do those things, and the movement is largely involuntary. These are small but constant movements, a bit like fidgeting. (It would be interesting to tape myself and actually quantify the amount of movement.)
It seems that one can induce an increase in NEAT, which is largely due to involuntary activities, by doing some voluntary things like placing a pillow on a chair or working while standing up.
Is it possible that the unnaturalness of comfy furniture, and particularly of comfy chairs, is contributing (together with other factors) to not only making us fat but also having low-back problems?
Both obesity and low-back problems are widespread among modern urbanites. Yet, from an evolutionary perspective, they should not be. They likely impaired survival success among our ancestors, and thus impaired their reproductive success. Evolution “gets angry” at these things; over time it wipes them out. In my reading of studies of hunter-gatherers, I don’t recall a single instance in which obesity and low-back problems were described as being widespread.
We’ve heard a lot about Big Society over the last few months, but what does it mean for the Arts/Health agenda in the North West?
We’re planning an event at Manchester Metropolitan University on the 29th October 2010.
This will follow on from last years North West Frontier, where health professionals, artists and other actors from the field fed into the start of a regional/sub-regional conversation around inequalities, the arts, health and well-being.
Aspirations from this event included; networking opportunities; access to wider networks and knowledge; training and advocacy.
We also discussed a strategic framework for the region, but with government changes, ongoing structural changes across all sectors and now vicious cuts, creating another strategy seems a futile exercise.
Following feedback from the networking sessions and dialogue across the region, what we’d be interested in doing is spending time together and creatively pulling together a Manifesto for Arts/Health across the region.
So this isn’t necessarily about frameworks, bullet-points and strategy; but it will be a statement about shared vision, passion, commitment and possibility that we and key allies can sign up to.
If you want to take part, places will be very limited and details will be forthcoming, but for now email artsforhealth@mmu.ac.uk to express your interest in taking part.
We’re planning an event at Manchester Metropolitan University on the 29th October 2010.
This will follow on from last years North West Frontier, where health professionals, artists and other actors from the field fed into the start of a regional/sub-regional conversation around inequalities, the arts, health and well-being.
Aspirations from this event included; networking opportunities; access to wider networks and knowledge; training and advocacy.
We also discussed a strategic framework for the region, but with government changes, ongoing structural changes across all sectors and now vicious cuts, creating another strategy seems a futile exercise.
Following feedback from the networking sessions and dialogue across the region, what we’d be interested in doing is spending time together and creatively pulling together a Manifesto for Arts/Health across the region.
So this isn’t necessarily about frameworks, bullet-points and strategy; but it will be a statement about shared vision, passion, commitment and possibility that we and key allies can sign up to.
If you want to take part, places will be very limited and details will be forthcoming, but for now email artsforhealth@mmu.ac.uk to express your interest in taking part.
Tuesday, September 21, 2010
REVIEW #7: Desert Essence Lemon Tea Tree Shampoo

NOTE: I am not paid to review this and other products. All products are purchased out of my own pocket and curiosity.
Purpose: Thoroughly cleanse scalp and hair without stripping of all the natural oils. (Recommended for oily scalp/hair. Try other flavors for dry scalp/hair.)
Ingredients: Aqueous Infusion of Certified Organic Extract of Citrus Medica Limonum (Lemon) Fruit (2), Cocoamidopropyl Betaine*, Sodium Coco-Sulfate*, Coco-Glucoside**, Polyquaternium-7*, Panthenol, Certified Organic Simmondsia Chinensis (Jojoba) Seed Oil (1), Leptospermum Petersonii Oil, Certified Organic Melaleuca Alternifolia (Tea Tree) Leaf Oil (1), Citric Acid, Sodium Chloride, Potassium Sorbate, Phenoxyethanol, Potassium Gluconate.1 Certified Organic by QAI 2 Certified Organic by QCS * Derived from Coconut **Derived from Sugar
Number of trials: Endless
How I use it:
• Rinse my hair under lukewarm water for 1-2 minutes
• Apply diluted shampoo to scalp ONLY using a color applicator bottle
• Massage my scalp and roots for 5 minutes then rinse
THE REVIEW:
My favorite characteristics about this shampoo are the natural ingredients, thorough yet gentle cleansing, and lathering capacity. In my transition to more natural shampoos, I've had a difficult time finding one that lathers and cleanses well ... until I met Desert Essence Lemon Tea Tree Shampoo. It works like a sulfate shampoo but without the harshness and dryness. It also pH-balanced according to my home test with litmus paper - about 6-7. Additionally, it leaves no residue and the scent is not overpowering. Though the product is expensive, I find that a little goes a long way.
PROS: lathers, thorough yet gentle cleanse, contains no EDTA (for you environmentalists), no SLS (if you're a sulfate-free fanatic), a little goes a long way, pH 6-7
CONS: expensive ($8.99 for 8 oz; you may find it for half that if you really hunt online)
RATING: Overall, I give the Desert Essence Lemon Tea Tree Shampoo 3 out of 5 stars because of the price. If I can find it for cheaper, I'd give it a full 5 stars.
Monday, September 20, 2010
The PriceWaterHouseCoopers 180 Conference
The PWC 180 Conference is an invitation only annual event in Washington DC. I was lucky enough to attend this years event at the "W" hotel in downtown DC, just across from the Treasury building. The opening event featured a panel conversation with notable figures like Malcolm Gladwell, Eric Topol and Esther Dyson, among others. The theme really struck home with me, namely, connecting with the healthcare consumer of the future. Are you a quantifiable selfer?? Do you measure your sleep brain waves with a ZEO and email the results to all of your friends?? Do you compete on line regarding how many miles you swim each day or how tough your morning workout really is?? Apparently, lots of top people in our field do this sort of thing as a matter of routine. We know from solid research that if your friends are healthy, you probably are too and the opposite is also true.I believe we have a lot more to learn about how best to change behavior and this conference gave me some good insights about the work involved. I am not quite ready to broadcast my REM sleep pattern but I am ready to compare workouts and my best running times too---especially if it will inspire others to adopt a healthy lifestyle. Promoting population health is what our school is all about and the PWC 180 Conference gave me all kinds of new ideas. Are you a quantifiable selfer--I did not even recognize the term until a week ago!!! DAVID NASH
Friday, September 17, 2010
Strong causation can exist without any correlation: The strange case of the chain smokers, and a note about diet
Researchers like to study samples of data and look for associations between variables. Often those associations are represented in the form of correlation coefficients, which go from -1 to 1. Another popular measure of association is the path coefficient, which usually has a narrower range of variation. What many researchers seem to forget is that the associations they find depend heavily on the sample they are looking at, and on the ranges of variation of the variables being analyzed.
A forgotten warning: Causation without correlation
Often those who conduct multivariate statistical analyses on data are unaware of certain limitations. Many times this is due to lack of familiarity with statistical tests. One warning we do see a lot though is: Correlation does not imply causation. This is, of course, absolutely true. If you take my weight from 1 to 20 years of age, and the price of gasoline in the US during that period, you will find that they are highly correlated. But common sense tells me that there is no causation whatsoever between these two variables.
So correlation does not imply causation alright, but there is another warning that is rarely seen: There can be strong causation without any correlation. Of course this can lead to even more bizarre conclusions than the “correlation does not imply causation” problem. If there is strong causation between variables B and Y, and it is not showing as a correlation, another variable A may “jump in” and “steal” that “unused correlation”; so to speak.
The chain smokers “study”
To illustrate this point, let us consider the following fictitious case, a study of “100 cities”. The study focuses on the effect of smoking and genes on lung cancer mortality. Smoking significantly increases the chances of dying from lung cancer; it is a very strong causative factor. Here are a few more details. Between 35 and 40 percent of the population are chain smokers. And there is a genotype (a set of genes), found in a small percentage of the population (around 7 percent), which is protective against lung cancer. All of those who are chain smokers die from lung cancer unless they die from other causes (e.g., accidents). Dying from other causes is a lot more common among those who have the protective genotype.
(I created this fictitious data with these associations in mind, using equations. I also added uncorrelated error into the equations, to make the data look a bit more realistic. For example, random deaths occurring early in life would reduce slightly any numeric association between chain smoking and cancer deaths in the sample of 100 cities.)
The table below shows part of the data, and gives an idea of the distribution of percentage of smokers (Smokers), percentage with the protective genotype (Pgenotype), and percentage of lung cancer deaths (MLCancer). (Click on it to enlarge. Use the "CRTL" and "+" keys to zoom in, and CRTL" and "-" to zoom out.) Each row corresponds to a city. The rest of the data, up to row 100, has a similar distribution.
The graphs below show the distribution of lung cancer deaths against: (a) the percentage of smokers, at the top; and (b) the percentage with the protective genotype, at the bottom. Correlations are shown at the top of each graph. (They can vary from -1 to 1. The closer they are to -1 or 1, the stronger is the association, negative or positive, between the variables.) The correlation between lung cancer deaths and percentage of smokers is slightly negative and statistically insignificant (-0.087). The correlation between lung cancer deaths and percentage with the protective genotype is negative, strong, and statistically significant (-0.613).
Even though smoking significantly increases the chances of dying from lung cancer, the correlations tell us otherwise. The correlations tell us that lung cancer does not seem to cause lung cancer deaths, and that having the protective genotype seems to significantly decrease cancer deaths. Why?
If there is no variation, there is no correlation
The reason is that the “researchers” collected data only about chain smokers. That is, the variable “Smokers” includes only chain smokers. If this was not a fictitious case, focusing the study on chain smokers could be seen as a clever strategy employed by researchers funded by tobacco companies. The researchers could say something like this: “We focused our analysis on those most likely to develop lung cancer.” Or, this could have been the result of plain stupidity when designing the research project.
By restricting their study to chain smokers the researchers dramatically reduced the variability in one particular variable: the extent to which the study participants smoked. Without variation, there can be no correlation. No matter what statistical test or software is used, no significant association will be found between lung cancer deaths and percentage of smokers based on this dataset. No matter what statistical test or software is used, a significant and strong association will be found between lung cancer deaths and percentage with the protective genotype.
Of course, this could lead to a very misleading conclusion. Smoking does not cause lung cancer; the real cause is genetic.
A note about diet
Consider the analogy between smoking and consumption of a particular food, and you will probably see what this means for the analysis of observational data regarding dietary choices and disease. This applies to almost any observational study, including the China Study. (Studies employing experimental control manipulations would presumably ensure enough variation in the variables studied.) In the China Study, data from dozens of counties were collected. One may find a significant association between consumption of food A and disease Y.
There may be a much stronger association between food B and disease Y, but that association may not show up in statistical analyses at all, simply because there is little variation in the data regarding consumption of food B. For example, all those sampled may have eaten food B; about the same amount. Or none. Or somewhere in between, within a rather small range of variation.
Statistical illiteracy, bad choices, and taxation
Statistics is a “necessary evil”. It is useful to go from small samples to large ones when we study any possible causal association. By doing so, one can find out whether an observed effect really applies to a larger percentage of the population, or is actually restricted to a small group of individuals. The problem is that we humans are very bad at inferring actual associations from simply looking at large tables with numbers. We need statistical tests for that.
However, ignorance about basic statistical phenomena, such as the one described here, can be costly. A group of people may eliminate food A from their diet based on coefficients of association resulting from what seem to be very clever analyses, replacing it with food B. The problem is that food B may be equally harmful, or even more harmful. And, that effect may not show up on statistical analyses unless they have enough variation in the consumption of food B.
Readers of this blog may wonder why we explicitly use terms like “suggests” when we refer to a relationship that is suggested by a significant coefficient of association (e.g., a linear correlation). This is why, among other reasons.
One does not have to be a mathematician to understand basic statistical concepts. And doing so can be very helpful in one’s life in general, not only in diet and lifestyle decisions. Even in simple choices, such as what to be on. We are always betting on something. For example, any investment is essentially a bet. Some outcomes are much more probable than others.
Once I had an interesting conversation with a high-level officer of a state government. I was part of a consulting team working on an information technology project. We were talking about the state lottery, which was a big source of revenue for the state, comparing it with state taxes. He told me something to this effect:
Our lottery is essentially a tax on the statistically illiterate.
A forgotten warning: Causation without correlation
Often those who conduct multivariate statistical analyses on data are unaware of certain limitations. Many times this is due to lack of familiarity with statistical tests. One warning we do see a lot though is: Correlation does not imply causation. This is, of course, absolutely true. If you take my weight from 1 to 20 years of age, and the price of gasoline in the US during that period, you will find that they are highly correlated. But common sense tells me that there is no causation whatsoever between these two variables.
So correlation does not imply causation alright, but there is another warning that is rarely seen: There can be strong causation without any correlation. Of course this can lead to even more bizarre conclusions than the “correlation does not imply causation” problem. If there is strong causation between variables B and Y, and it is not showing as a correlation, another variable A may “jump in” and “steal” that “unused correlation”; so to speak.
The chain smokers “study”
To illustrate this point, let us consider the following fictitious case, a study of “100 cities”. The study focuses on the effect of smoking and genes on lung cancer mortality. Smoking significantly increases the chances of dying from lung cancer; it is a very strong causative factor. Here are a few more details. Between 35 and 40 percent of the population are chain smokers. And there is a genotype (a set of genes), found in a small percentage of the population (around 7 percent), which is protective against lung cancer. All of those who are chain smokers die from lung cancer unless they die from other causes (e.g., accidents). Dying from other causes is a lot more common among those who have the protective genotype.
(I created this fictitious data with these associations in mind, using equations. I also added uncorrelated error into the equations, to make the data look a bit more realistic. For example, random deaths occurring early in life would reduce slightly any numeric association between chain smoking and cancer deaths in the sample of 100 cities.)
The table below shows part of the data, and gives an idea of the distribution of percentage of smokers (Smokers), percentage with the protective genotype (Pgenotype), and percentage of lung cancer deaths (MLCancer). (Click on it to enlarge. Use the "CRTL" and "+" keys to zoom in, and CRTL" and "-" to zoom out.) Each row corresponds to a city. The rest of the data, up to row 100, has a similar distribution.
The graphs below show the distribution of lung cancer deaths against: (a) the percentage of smokers, at the top; and (b) the percentage with the protective genotype, at the bottom. Correlations are shown at the top of each graph. (They can vary from -1 to 1. The closer they are to -1 or 1, the stronger is the association, negative or positive, between the variables.) The correlation between lung cancer deaths and percentage of smokers is slightly negative and statistically insignificant (-0.087). The correlation between lung cancer deaths and percentage with the protective genotype is negative, strong, and statistically significant (-0.613).
Even though smoking significantly increases the chances of dying from lung cancer, the correlations tell us otherwise. The correlations tell us that lung cancer does not seem to cause lung cancer deaths, and that having the protective genotype seems to significantly decrease cancer deaths. Why?
If there is no variation, there is no correlation
The reason is that the “researchers” collected data only about chain smokers. That is, the variable “Smokers” includes only chain smokers. If this was not a fictitious case, focusing the study on chain smokers could be seen as a clever strategy employed by researchers funded by tobacco companies. The researchers could say something like this: “We focused our analysis on those most likely to develop lung cancer.” Or, this could have been the result of plain stupidity when designing the research project.
By restricting their study to chain smokers the researchers dramatically reduced the variability in one particular variable: the extent to which the study participants smoked. Without variation, there can be no correlation. No matter what statistical test or software is used, no significant association will be found between lung cancer deaths and percentage of smokers based on this dataset. No matter what statistical test or software is used, a significant and strong association will be found between lung cancer deaths and percentage with the protective genotype.
Of course, this could lead to a very misleading conclusion. Smoking does not cause lung cancer; the real cause is genetic.
A note about diet
Consider the analogy between smoking and consumption of a particular food, and you will probably see what this means for the analysis of observational data regarding dietary choices and disease. This applies to almost any observational study, including the China Study. (Studies employing experimental control manipulations would presumably ensure enough variation in the variables studied.) In the China Study, data from dozens of counties were collected. One may find a significant association between consumption of food A and disease Y.
There may be a much stronger association between food B and disease Y, but that association may not show up in statistical analyses at all, simply because there is little variation in the data regarding consumption of food B. For example, all those sampled may have eaten food B; about the same amount. Or none. Or somewhere in between, within a rather small range of variation.
Statistical illiteracy, bad choices, and taxation
Statistics is a “necessary evil”. It is useful to go from small samples to large ones when we study any possible causal association. By doing so, one can find out whether an observed effect really applies to a larger percentage of the population, or is actually restricted to a small group of individuals. The problem is that we humans are very bad at inferring actual associations from simply looking at large tables with numbers. We need statistical tests for that.
However, ignorance about basic statistical phenomena, such as the one described here, can be costly. A group of people may eliminate food A from their diet based on coefficients of association resulting from what seem to be very clever analyses, replacing it with food B. The problem is that food B may be equally harmful, or even more harmful. And, that effect may not show up on statistical analyses unless they have enough variation in the consumption of food B.
Readers of this blog may wonder why we explicitly use terms like “suggests” when we refer to a relationship that is suggested by a significant coefficient of association (e.g., a linear correlation). This is why, among other reasons.
One does not have to be a mathematician to understand basic statistical concepts. And doing so can be very helpful in one’s life in general, not only in diet and lifestyle decisions. Even in simple choices, such as what to be on. We are always betting on something. For example, any investment is essentially a bet. Some outcomes are much more probable than others.
Once I had an interesting conversation with a high-level officer of a state government. I was part of a consulting team working on an information technology project. We were talking about the state lottery, which was a big source of revenue for the state, comparing it with state taxes. He told me something to this effect:
Our lottery is essentially a tax on the statistically illiterate.
Thursday, September 16, 2010
Guest Commentary: Interpreting Healthcare Budget Projections
Joe Couto, PharmD, MBA
Outcomes Research Fellowship Director
Jefferson School of Population Health
Last week, media outlets were abuzz from a Health Affairs article that was published online that showed a slight increase in the growth of US aggregate health spending (0.2%) compared to an analysis published in March’s issue prior to the passage of reform. Yearly, this report is authored by the Office of the Actuary at the Centers for Medicare and Medicaid Services (CMS) and published in the journal with little fanfare.
However, in light of the controversy surrounding healthcare reform and mid-term elections, this report was touted by political pundits as yet more proof that healthcare reform is already a failed experiment. Their contention is that, contrary to the claim in March 2010 by the nonpartisan Congressional Budget Office (CBO) that the legislation would result in a net budgetary savings of $143 billion over the period 2010-2019, the legislation will instead grow healthcare costs over this period. While there is a bit of truth to their claim, a lot of facts have been left out of their reporting.
First, these projections have been made by different agencies, with CMS the source of the Health Affairs article, and the CBO the source of the figure often quoted by the Obama administration. Therefore variation is to be expected.
Second, the two figures are not directly comparable. The CBO’s figure is merely based on what the government will pay for healthcare over the next 10 years, most notably Medicare and Medicaid. The CMS figure of national health spending growth includes both public and private payers, and actually projects no increase in the growth of government spending on healthcare under the new health reform law. Thus the 0.2% increase in national health spending is attributed to growth in spending on the private payer side of the equation. This is explicitly demonstrated in the tables published in the Health Affairs article.
It is also important to note that in late August 2010 the Director of the CBO, Douglas Elmendorf, stated in a letter to Sen. Crapo (R-Idaho) that he has no reason to believe that his agencies’ projections from March would differ substantially 5 months later.
Third, it is important to realize that budget predictions are historically inaccurate and subject to sizeable variation. In 2002, CMS projected US aggregate health spending to grow at a rate of 6.7% in years 2009 – 2011. In 2008, growth was projected to be 6.6% and 6.7% during this period. The current CMS projections estimate spending to grow at rates of 5.8% (2009), 5.1% (2010), and 4.2% (2011). Thus a change of 0.2% would seem relatively insignificant in light of the variation seen over time in these projections. The authors of the latest Health Affairs article recognize that “many facets of these projections could change dramatically” over time.
Finally, the primary goal of health reform legislation was not to control cost, but to expand coverage. While it starts to create a more efficient system where costs can theoretically be controlled over time, the legislation does not contain many provisions whose sole focus is to control or contain costs.
What escaped the majority of authors of the editorials that appeared in the lay press last week is that the Health Affairs article underscored the fact that this legislation will cover an additional 32.5 million Americans by 2019 (9.7% of the US population in 2019), with little projected impact on health spending growth over the next 10 years. No matter what side of the political fence you sit on, this is truly extraordinary.
Outcomes Research Fellowship Director
Jefferson School of Population Health
Last week, media outlets were abuzz from a Health Affairs article that was published online that showed a slight increase in the growth of US aggregate health spending (0.2%) compared to an analysis published in March’s issue prior to the passage of reform. Yearly, this report is authored by the Office of the Actuary at the Centers for Medicare and Medicaid Services (CMS) and published in the journal with little fanfare.
However, in light of the controversy surrounding healthcare reform and mid-term elections, this report was touted by political pundits as yet more proof that healthcare reform is already a failed experiment. Their contention is that, contrary to the claim in March 2010 by the nonpartisan Congressional Budget Office (CBO) that the legislation would result in a net budgetary savings of $143 billion over the period 2010-2019, the legislation will instead grow healthcare costs over this period. While there is a bit of truth to their claim, a lot of facts have been left out of their reporting.
First, these projections have been made by different agencies, with CMS the source of the Health Affairs article, and the CBO the source of the figure often quoted by the Obama administration. Therefore variation is to be expected.
Second, the two figures are not directly comparable. The CBO’s figure is merely based on what the government will pay for healthcare over the next 10 years, most notably Medicare and Medicaid. The CMS figure of national health spending growth includes both public and private payers, and actually projects no increase in the growth of government spending on healthcare under the new health reform law. Thus the 0.2% increase in national health spending is attributed to growth in spending on the private payer side of the equation. This is explicitly demonstrated in the tables published in the Health Affairs article.
It is also important to note that in late August 2010 the Director of the CBO, Douglas Elmendorf, stated in a letter to Sen. Crapo (R-Idaho) that he has no reason to believe that his agencies’ projections from March would differ substantially 5 months later.
Third, it is important to realize that budget predictions are historically inaccurate and subject to sizeable variation. In 2002, CMS projected US aggregate health spending to grow at a rate of 6.7% in years 2009 – 2011. In 2008, growth was projected to be 6.6% and 6.7% during this period. The current CMS projections estimate spending to grow at rates of 5.8% (2009), 5.1% (2010), and 4.2% (2011). Thus a change of 0.2% would seem relatively insignificant in light of the variation seen over time in these projections. The authors of the latest Health Affairs article recognize that “many facets of these projections could change dramatically” over time.
Finally, the primary goal of health reform legislation was not to control cost, but to expand coverage. While it starts to create a more efficient system where costs can theoretically be controlled over time, the legislation does not contain many provisions whose sole focus is to control or contain costs.
What escaped the majority of authors of the editorials that appeared in the lay press last week is that the Health Affairs article underscored the fact that this legislation will cover an additional 32.5 million Americans by 2019 (9.7% of the US population in 2019), with little projected impact on health spending growth over the next 10 years. No matter what side of the political fence you sit on, this is truly extraordinary.
Monday, September 13, 2010
Guest Commentary: JSPH's New Online Degree Programs

Juan Leon, PhD
Director of Online Learning
Jefferson School of Population Health

Lisa Chosed, MA
Online Programs Administrative Liaison
Jefferson School of Population Health
Jefferson School of Population Health (JSPH) academic degree programs are now online!
Juan Leon, Director of Online Learning, and Lisa Chosed, Online Programs Administrative Liaison, have been working since January to provide support to the first cohort of faculty who will be teaching online.
Students taking online courses receive an Online Student Orientation—6 hours of training that acclimates newcomers to the structure of the online courses and the online environment in general. The course ensures that online students are familiar with JSPH academic policies and have access to all of the same resources as on-site students. The Orientation also introduces fundamental online skills such as conducting literature searches in the library, posting assignments, and producing papers in conformance with style guidelines. Our Master of Science degrees in Health Policy, Chronic Care Management, and Healthcare Quality & Safety are completely online...and courses go live Monday morning, September 13th at 9:00AM. We are excited and ready!
How do our online programs fit into the broader educational landscape today? According to a report released last year by the Sloan Consortium (Sloan-C), a leading research center, online enrollments continue to grow faster than those for the entire higher education student population. More than 1 in 4 higher education students today take at least one course online.
While offering online programs is in keeping with the larger national trends, we are the first to offer online Master’s degrees in Healthcare Quality and Safety and in Chronic Care Management. Other distinguishing features of our programs are the small, specialized courses, highly qualified faculty, and the strongly motivated student body comprised of professionals in health care and related careers. Our students are finding that online courses can fit into their busy schedules, and that our focus on workplace applications of learning allows them to implement positive changes, both immediately and over the longer term.
The Sloan-C report, “Learning On Demand: Online Education in the United States, 2009,” is available here.
What's Your FALL Regimen?
With Autumn around the corner, will you adjust your hair care regimen? If so, what changes will you make? Longer protective styles? Fewer washes? ...
Loo's SUMMER Regimen
•Prepoo, Wash, and DC every 1-2 weeks
•Airdry
•Twist every 2-3 weeks
•Moisturize weekly
Loo's FALL Regimen
•Prepoo, Wash, and DC every 2-3 weeks
•Airdry
•Twist every 3-4 weeks
•Moisturize weekly
Loo's SUMMER Regimen
•Prepoo, Wash, and DC every 1-2 weeks
•Airdry
•Twist every 2-3 weeks
•Moisturize weekly
Loo's FALL Regimen
•Prepoo, Wash, and DC every 2-3 weeks
•Airdry
•Twist every 3-4 weeks
•Moisturize weekly
Kojic Acid: Natural Alternative against Hyperpigmentation
Mushroom extract. Used effectively to lighten dark spots.
MORE ABOUT KOJIC ACID
WEBMD ON KOJIC ACID #1
WEBMD ON KOJIC ACID #2
MORE ABOUT KOJIC ACID
WEBMD ON KOJIC ACID #1
WEBMD ON KOJIC ACID #2
Labels:
Skin Care
Sunday, September 12, 2010
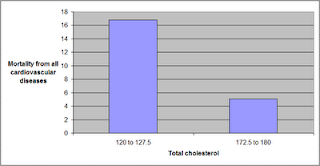
The China Study II: Wheat flour, rice, and cardiovascular disease
In my last post on the China Study II, I analyzed the effect of total and HDL cholesterol on mortality from all cardiovascular diseases. The main conclusion was that total and HDL cholesterol were protective. Total and HDL cholesterol usually increase with intake of animal foods, and particularly of animal fat. The lowest mortality from all cardiovascular diseases was in the highest total cholesterol range, 172.5 to 180; and the highest mortality in the lowest total cholesterol range, 120 to 127.5. The difference was quite large; the mortality in the lowest range was approximately 3.3 times higher than in the highest.
This post focuses on the intake of two main plant foods, namely wheat flour and rice intake, and their relationships with mortality from all cardiovascular diseases. After many exploratory multivariate analyses, wheat flour and rice emerged as the plant foods with the strongest associations with mortality from all cardiovascular diseases. Moreover, wheat flour and rice have a strong and inverse relationship with each other, which suggests a “consumption divide”. Since the data is from China in the late 1980s, it is likely that consumption of wheat flour is even higher now. As you’ll see, this picture is alarming.
The main model and results
All of the results reported here are from analyses conducted using WarpPLS. Below is the model with the main results of the analyses. (Click on it to enlarge. Use the "CRTL" and "+" keys to zoom in, and CRTL" and "-" to zoom out.) The arrows explore associations between variables, which are shown within ovals. The meaning of each variable is the following: SexM1F2 = sex, with 1 assigned to males and 2 to females; MVASC = mortality from all cardiovascular diseases (ages 35-69); TKCAL = total calorie intake per day; WHTFLOUR = wheat flour intake (g/day); and RICE = and rice intake (g/day).
The variables to the left of MVASC are the main predictors of interest in the model. The one to the right is a control variable – SexM1F2. The path coefficients (indicated as beta coefficients) reflect the strength of the relationships. A negative beta means that the relationship is negative; i.e., an increase in a variable is associated with a decrease in the variable that it points to. The P values indicate the statistical significance of the relationship; a P lower than 0.05 generally means a significant relationship (95 percent or higher likelihood that the relationship is “real”).
In summary, the model above seems to be telling us that:
- As rice intake increases, wheat flour intake decreases significantly (beta=-0.84; P<0.01). This relationship would be the same if the arrow pointed in the opposite direction. It suggests that there is a sharp divide between rice-consuming and wheat flour-consuming regions.
- As wheat flour intake increases, mortality from all cardiovascular diseases increases significantly (beta=0.32; P<0.01). This is after controlling for the effects of rice and total calorie intake. That is, wheat flour seems to have some inherent properties that make it bad for one’s health, even if one doesn’t consume that many calories.
- As rice intake increases, mortality from all cardiovascular diseases decreases significantly (beta=-0.24; P<0.01). This is after controlling for the effects of wheat flour and total calorie intake. That is, this effect is not entirely due to rice being consumed in place of wheat flour. Still, as you’ll see later in this post, this relationship is nonlinear. Excessive rice intake does not seem to be very good for one’s health either.
- Increases in wheat flour and rice intake are significantly associated with increases in total calorie intake (betas=0.25, 0.33; P<0.01). This may be due to wheat flour and rice intake: (a) being themselves, in terms of their own caloric content, main contributors to the total calorie intake; or (b) causing an increase in calorie intake from other sources. The former is more likely, given the effect below.
- The effect of total calorie intake on mortality from all cardiovascular diseases is insignificant when we control for the effects of rice and wheat flour intakes (beta=0.08; P=0.35). This suggests that neither wheat flour nor rice exerts an effect on mortality from all cardiovascular diseases by increasing total calorie intake from other food sources.
- Being female is significantly associated with a reduction in mortality from all cardiovascular diseases (beta=-0.24; P=0.01). This is to be expected. In other words, men are women with a few design flaws, so to speak. (This situation reverses itself a bit after menopause.)
Wheat flour displaces rice
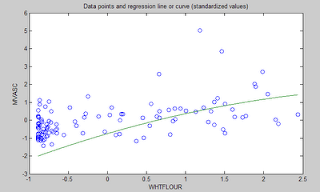
The graph below shows the shape of the association between wheat flour intake (WHTFLOUR) and rice intake (RICE). The values are provided in standardized format; e.g., 0 is the mean (a.k.a. average), 1 is one standard deviation above the mean, and so on. The curve is the best-fitting U curve obtained by the software. It actually has the shape of an exponential decay curve, which can be seen as a section of a U curve. This suggests that wheat flour consumption has strongly displaced rice consumption in several regions in China, and also that wherever rice consumption is high wheat flour consumption tends to be low.
As wheat flour intake goes up, so does cardiovascular disease mortality
The graphs below show the shapes of the association between wheat flour intake (WHTFLOUR) and mortality from all cardiovascular diseases (MVASC). In the first graph, the values are provided in standardized format; e.g., 0 is the mean (or average), 1 is one standard deviation above the mean, and so on. In the second graph, the values are provided in unstandardized format and organized in terciles (each of three equal intervals).
The curve in the first graph is the best-fitting U curve obtained by the software. It is a quasi-linear relationship. The higher the consumption of wheat flour in a county, the higher seems to be the mortality from all cardiovascular diseases. The second graph suggests that mortality in the third tercile, which represents a consumption of wheat flour of 501 to 751 g/day (a lot!), is 69 percent higher than mortality in the first tercile (0 to 251 g/day).
Rice seems to be protective, as long as intake is not too high
The graphs below show the shapes of the association between rice intake (RICE) and mortality from all cardiovascular diseases (MVASC). In the first graph, the values are provided in standardized format. In the second graph, the values are provided in unstandardized format and organized in terciles.
Here the relationship is more complex. The lowest mortality is clearly in the second tercile (206 to 412 g/day). There is a lot of variation in the first tercile, as suggested by the first graph with the U curve. (Remember, as rice intake goes down, wheat flour intake tends to go up.) The U curve here looks similar to the exponential decay curve shown earlier in the post, for the relationship between rice and wheat flour intake.
In fact, the shape of the association between rice intake and mortality from all cardiovascular diseases looks a bit like an “echo” of the shape of the relationship between rice and wheat flour intake. Here is what is creepy. This echo looks somewhat like the first curve (between rice and wheat flour intake), but with wheat flour intake replaced by “death” (i.e., mortality from all cardiovascular diseases).
What does this all mean?
- Wheat flour displacing rice does not look like a good thing. Wheat flour intake seems to have strongly displaced rice intake in the counties where it is heavily consumed. Generally speaking, that does not seem to have been a good thing. It looks like this is generally associated with increased mortality from all cardiovascular diseases.
- High glycemic index food consumption does not seem to be the problem here. Wheat flour and rice have very similar glycemic indices (but generally not glycemic loads; see below). Both lead to blood glucose and insulin spikes. Yet, rice consumption seems protective when it is not excessive. This is true in part (but not entirely) because it largely displaces wheat flour. Moreover, neither rice nor wheat flour consumption seems to be significantly associated with cardiovascular disease via an increase in total calorie consumption. This is a bit of a blow to the theory that high glycemic carbohydrates necessarily cause obesity, diabetes, and eventually cardiovascular disease.
- The problem with wheat flour is … hard to pinpoint, based on the results summarized here. Maybe it is the fact that it is an ultra-refined carbohydrate-rich food; less refined forms of wheat could be healthier. In fact, the glycemic loads of less refined carbohydrate-rich foods tend to be much lower than those of more refined ones. (Also, boiled brown rice has a glycemic load that is about three times lower than that of whole wheat bread; whereas the glycemic indices are about the same.) Maybe the problem is wheat flour's gluten content. Maybe it is a combination of various factors, including these.
Reference
Kock, N. (2010). WarpPLS 1.0 User Manual. Laredo, Texas: ScriptWarp Systems.
Acknowledgment and notes
- Many thanks are due to Dr. Campbell and his collaborators for collecting and compiling the data used in this analysis. The data is from this site, created by those researchers to disseminate their work in connection with a study often referred to as the “China Study II”. It has already been analyzed by other bloggers. Notable analyses have been conducted by Ricardo at Canibais e Reis, Stan at Heretic, and Denise at Raw Food SOS.
- The path coefficients (indicated as beta coefficients) reflect the strength of the relationships; they are a bit like standard univariate (or Pearson) correlation coefficients, except that they take into consideration multivariate relationships (they control for competing effects on each variable). Whenever nonlinear relationships were modeled, the path coefficients were automatically corrected by the software to account for nonlinearity.
- The software used here identifies non-cyclical and mono-cyclical relationships such as logarithmic, exponential, and hyperbolic decay relationships. Once a relationship is identified, data values are corrected and coefficients calculated. This is not the same as log-transforming data prior to analysis, which is widely used but only works if the underlying relationship is logarithmic. Otherwise, log-transforming data may distort the relationship even more than assuming that it is linear, which is what is done by most statistical software tools.
- The R-squared values reflect the percentage of explained variance for certain variables; the higher they are, the better the model fit with the data. In complex and multi-factorial phenomena such as health-related phenomena, many would consider an R-squared of 0.20 as acceptable. Still, such an R-squared would mean that 80 percent of the variance for a particularly variable is unexplained by the data.
- The P values have been calculated using a nonparametric technique, a form of resampling called jackknifing, which does not require the assumption that the data is normally distributed to be met. This and other related techniques also tend to yield more reliable results for small samples, and samples with outliers (as long as the outliers are “good” data, and are not the result of measurement error).
- Only two data points per county were used (for males and females). This increased the sample size of the dataset without artificially reducing variance, which is desirable since the dataset is relatively small. This also allowed for the test of commonsense assumptions (e.g., the protective effects of being female), which is always a good idea in a complex analysis because violation of commonsense assumptions may suggest data collection or analysis error. On the other hand, it required the inclusion of a sex variable as a control variable in the analysis, which is no big deal.
- Since all the data was collected around the same time (late 1980s), this analysis assumes a somewhat static pattern of consumption of rice and wheat flour. In other words, let us assume that variations in consumption of a particular food do lead to variations in mortality. Still, that effect will typically take years to manifest itself. This is a major limitation of this dataset and any related analyses.
- Mortality from schistosomiasis infection (MSCHIST) does not confound the results presented here. Only counties where no deaths from schistosomiasis infection were reported have been included in this analysis. Mortality from all cardiovascular diseases (MVASC) was measured using the variable M059 ALLVASCc (ages 35-69). See this post for other notes that apply here as well.
This post focuses on the intake of two main plant foods, namely wheat flour and rice intake, and their relationships with mortality from all cardiovascular diseases. After many exploratory multivariate analyses, wheat flour and rice emerged as the plant foods with the strongest associations with mortality from all cardiovascular diseases. Moreover, wheat flour and rice have a strong and inverse relationship with each other, which suggests a “consumption divide”. Since the data is from China in the late 1980s, it is likely that consumption of wheat flour is even higher now. As you’ll see, this picture is alarming.
The main model and results
All of the results reported here are from analyses conducted using WarpPLS. Below is the model with the main results of the analyses. (Click on it to enlarge. Use the "CRTL" and "+" keys to zoom in, and CRTL" and "-" to zoom out.) The arrows explore associations between variables, which are shown within ovals. The meaning of each variable is the following: SexM1F2 = sex, with 1 assigned to males and 2 to females; MVASC = mortality from all cardiovascular diseases (ages 35-69); TKCAL = total calorie intake per day; WHTFLOUR = wheat flour intake (g/day); and RICE = and rice intake (g/day).
The variables to the left of MVASC are the main predictors of interest in the model. The one to the right is a control variable – SexM1F2. The path coefficients (indicated as beta coefficients) reflect the strength of the relationships. A negative beta means that the relationship is negative; i.e., an increase in a variable is associated with a decrease in the variable that it points to. The P values indicate the statistical significance of the relationship; a P lower than 0.05 generally means a significant relationship (95 percent or higher likelihood that the relationship is “real”).
In summary, the model above seems to be telling us that:
- As rice intake increases, wheat flour intake decreases significantly (beta=-0.84; P<0.01). This relationship would be the same if the arrow pointed in the opposite direction. It suggests that there is a sharp divide between rice-consuming and wheat flour-consuming regions.
- As wheat flour intake increases, mortality from all cardiovascular diseases increases significantly (beta=0.32; P<0.01). This is after controlling for the effects of rice and total calorie intake. That is, wheat flour seems to have some inherent properties that make it bad for one’s health, even if one doesn’t consume that many calories.
- As rice intake increases, mortality from all cardiovascular diseases decreases significantly (beta=-0.24; P<0.01). This is after controlling for the effects of wheat flour and total calorie intake. That is, this effect is not entirely due to rice being consumed in place of wheat flour. Still, as you’ll see later in this post, this relationship is nonlinear. Excessive rice intake does not seem to be very good for one’s health either.
- Increases in wheat flour and rice intake are significantly associated with increases in total calorie intake (betas=0.25, 0.33; P<0.01). This may be due to wheat flour and rice intake: (a) being themselves, in terms of their own caloric content, main contributors to the total calorie intake; or (b) causing an increase in calorie intake from other sources. The former is more likely, given the effect below.
- The effect of total calorie intake on mortality from all cardiovascular diseases is insignificant when we control for the effects of rice and wheat flour intakes (beta=0.08; P=0.35). This suggests that neither wheat flour nor rice exerts an effect on mortality from all cardiovascular diseases by increasing total calorie intake from other food sources.
- Being female is significantly associated with a reduction in mortality from all cardiovascular diseases (beta=-0.24; P=0.01). This is to be expected. In other words, men are women with a few design flaws, so to speak. (This situation reverses itself a bit after menopause.)
Wheat flour displaces rice
The graph below shows the shape of the association between wheat flour intake (WHTFLOUR) and rice intake (RICE). The values are provided in standardized format; e.g., 0 is the mean (a.k.a. average), 1 is one standard deviation above the mean, and so on. The curve is the best-fitting U curve obtained by the software. It actually has the shape of an exponential decay curve, which can be seen as a section of a U curve. This suggests that wheat flour consumption has strongly displaced rice consumption in several regions in China, and also that wherever rice consumption is high wheat flour consumption tends to be low.
As wheat flour intake goes up, so does cardiovascular disease mortality
The graphs below show the shapes of the association between wheat flour intake (WHTFLOUR) and mortality from all cardiovascular diseases (MVASC). In the first graph, the values are provided in standardized format; e.g., 0 is the mean (or average), 1 is one standard deviation above the mean, and so on. In the second graph, the values are provided in unstandardized format and organized in terciles (each of three equal intervals).
The curve in the first graph is the best-fitting U curve obtained by the software. It is a quasi-linear relationship. The higher the consumption of wheat flour in a county, the higher seems to be the mortality from all cardiovascular diseases. The second graph suggests that mortality in the third tercile, which represents a consumption of wheat flour of 501 to 751 g/day (a lot!), is 69 percent higher than mortality in the first tercile (0 to 251 g/day).
Rice seems to be protective, as long as intake is not too high
The graphs below show the shapes of the association between rice intake (RICE) and mortality from all cardiovascular diseases (MVASC). In the first graph, the values are provided in standardized format. In the second graph, the values are provided in unstandardized format and organized in terciles.
Here the relationship is more complex. The lowest mortality is clearly in the second tercile (206 to 412 g/day). There is a lot of variation in the first tercile, as suggested by the first graph with the U curve. (Remember, as rice intake goes down, wheat flour intake tends to go up.) The U curve here looks similar to the exponential decay curve shown earlier in the post, for the relationship between rice and wheat flour intake.
In fact, the shape of the association between rice intake and mortality from all cardiovascular diseases looks a bit like an “echo” of the shape of the relationship between rice and wheat flour intake. Here is what is creepy. This echo looks somewhat like the first curve (between rice and wheat flour intake), but with wheat flour intake replaced by “death” (i.e., mortality from all cardiovascular diseases).
What does this all mean?
- Wheat flour displacing rice does not look like a good thing. Wheat flour intake seems to have strongly displaced rice intake in the counties where it is heavily consumed. Generally speaking, that does not seem to have been a good thing. It looks like this is generally associated with increased mortality from all cardiovascular diseases.
- High glycemic index food consumption does not seem to be the problem here. Wheat flour and rice have very similar glycemic indices (but generally not glycemic loads; see below). Both lead to blood glucose and insulin spikes. Yet, rice consumption seems protective when it is not excessive. This is true in part (but not entirely) because it largely displaces wheat flour. Moreover, neither rice nor wheat flour consumption seems to be significantly associated with cardiovascular disease via an increase in total calorie consumption. This is a bit of a blow to the theory that high glycemic carbohydrates necessarily cause obesity, diabetes, and eventually cardiovascular disease.
- The problem with wheat flour is … hard to pinpoint, based on the results summarized here. Maybe it is the fact that it is an ultra-refined carbohydrate-rich food; less refined forms of wheat could be healthier. In fact, the glycemic loads of less refined carbohydrate-rich foods tend to be much lower than those of more refined ones. (Also, boiled brown rice has a glycemic load that is about three times lower than that of whole wheat bread; whereas the glycemic indices are about the same.) Maybe the problem is wheat flour's gluten content. Maybe it is a combination of various factors, including these.
Reference
Kock, N. (2010). WarpPLS 1.0 User Manual. Laredo, Texas: ScriptWarp Systems.
Acknowledgment and notes
- Many thanks are due to Dr. Campbell and his collaborators for collecting and compiling the data used in this analysis. The data is from this site, created by those researchers to disseminate their work in connection with a study often referred to as the “China Study II”. It has already been analyzed by other bloggers. Notable analyses have been conducted by Ricardo at Canibais e Reis, Stan at Heretic, and Denise at Raw Food SOS.
- The path coefficients (indicated as beta coefficients) reflect the strength of the relationships; they are a bit like standard univariate (or Pearson) correlation coefficients, except that they take into consideration multivariate relationships (they control for competing effects on each variable). Whenever nonlinear relationships were modeled, the path coefficients were automatically corrected by the software to account for nonlinearity.
- The software used here identifies non-cyclical and mono-cyclical relationships such as logarithmic, exponential, and hyperbolic decay relationships. Once a relationship is identified, data values are corrected and coefficients calculated. This is not the same as log-transforming data prior to analysis, which is widely used but only works if the underlying relationship is logarithmic. Otherwise, log-transforming data may distort the relationship even more than assuming that it is linear, which is what is done by most statistical software tools.
- The R-squared values reflect the percentage of explained variance for certain variables; the higher they are, the better the model fit with the data. In complex and multi-factorial phenomena such as health-related phenomena, many would consider an R-squared of 0.20 as acceptable. Still, such an R-squared would mean that 80 percent of the variance for a particularly variable is unexplained by the data.
- The P values have been calculated using a nonparametric technique, a form of resampling called jackknifing, which does not require the assumption that the data is normally distributed to be met. This and other related techniques also tend to yield more reliable results for small samples, and samples with outliers (as long as the outliers are “good” data, and are not the result of measurement error).
- Only two data points per county were used (for males and females). This increased the sample size of the dataset without artificially reducing variance, which is desirable since the dataset is relatively small. This also allowed for the test of commonsense assumptions (e.g., the protective effects of being female), which is always a good idea in a complex analysis because violation of commonsense assumptions may suggest data collection or analysis error. On the other hand, it required the inclusion of a sex variable as a control variable in the analysis, which is no big deal.
- Since all the data was collected around the same time (late 1980s), this analysis assumes a somewhat static pattern of consumption of rice and wheat flour. In other words, let us assume that variations in consumption of a particular food do lead to variations in mortality. Still, that effect will typically take years to manifest itself. This is a major limitation of this dataset and any related analyses.
- Mortality from schistosomiasis infection (MSCHIST) does not confound the results presented here. Only counties where no deaths from schistosomiasis infection were reported have been included in this analysis. Mortality from all cardiovascular diseases (MVASC) was measured using the variable M059 ALLVASCc (ages 35-69). See this post for other notes that apply here as well.
Thursday, September 9, 2010
Twist Series: Maintenance I
It's official! The twist series has begun. Today, I start by answering some of your questions. The remaining questions will be answered in the weeks to come ... Feel free to continue adding more questions/comments.
How long do you keep yours in?
2-3 weeks. I no longer keep them in for 4 weeks at a time since my current lifestyle requires that I look more "polished".
How many twists do you make?
About 40 twists on average. Sometimes 30, sometimes 55.
How large do you make them?
Medium to large. Sometimes I make them small. I no longer do jumbo since they don't last as long. I haven't had time for micro/mini twists since my last set. (My micro twists can be seen here.)
What products do you use?
On twist day, I start off with a Coconut Oil prepoo, followed by a wash with Desert Essence Lemon Tea Tree, followed by deep conditioning with Lekair Cholesterol. I then detangle before rinsing the conditioner. I airdry about 80-90% of the way in plaits. Then I apply a homemade Whipped Shea Butter to my whole head and begin twisting. (The whipped shea butter recipe can be found here.)
Do you do any daily/weekly/monthly maintenance?
Yes. I wear a satin scarf or bonnet nightly to keep the twists moisturized and intact. Before putting on the scarf/bonnet, I put my twists into a french roll or three big twists. (No bobby pins, ouchless bands, or anything; just hair.) Weekly, I spritz my hair with a little water ... just enough to make it slightly damp and no more than that. Then I reapply the whipped shea butter and wrap my hair with a satin scarf. If it is a wash week, I may redo the perimeter of my twists.
How do you keep your ends moisturized?
I spritz water and apply whipped shea butter weekly (unless it's a wash week). I then follow up by wrapping my hair with a satin scarf until it dries ... otherwise, it'll be frizz galore. Before wrapping my hair, I put my twists in a french roll or three big twists.
How often do you shampoo/condition your hair while it is twisted up?
About 1x every 1-3 weeks, depending on the season. I tend to wash more frequently in the summer versus the rest of the year. I tend to wash more frequently if I've been sweating or if my hair is extremely parched.
How long do you keep yours in?
2-3 weeks. I no longer keep them in for 4 weeks at a time since my current lifestyle requires that I look more "polished".
How many twists do you make?
About 40 twists on average. Sometimes 30, sometimes 55.
How large do you make them?
Medium to large. Sometimes I make them small. I no longer do jumbo since they don't last as long. I haven't had time for micro/mini twists since my last set. (My micro twists can be seen here.)
What products do you use?
On twist day, I start off with a Coconut Oil prepoo, followed by a wash with Desert Essence Lemon Tea Tree, followed by deep conditioning with Lekair Cholesterol. I then detangle before rinsing the conditioner. I airdry about 80-90% of the way in plaits. Then I apply a homemade Whipped Shea Butter to my whole head and begin twisting. (The whipped shea butter recipe can be found here.)
Do you do any daily/weekly/monthly maintenance?
Yes. I wear a satin scarf or bonnet nightly to keep the twists moisturized and intact. Before putting on the scarf/bonnet, I put my twists into a french roll or three big twists. (No bobby pins, ouchless bands, or anything; just hair.) Weekly, I spritz my hair with a little water ... just enough to make it slightly damp and no more than that. Then I reapply the whipped shea butter and wrap my hair with a satin scarf. If it is a wash week, I may redo the perimeter of my twists.
How do you keep your ends moisturized?
I spritz water and apply whipped shea butter weekly (unless it's a wash week). I then follow up by wrapping my hair with a satin scarf until it dries ... otherwise, it'll be frizz galore. Before wrapping my hair, I put my twists in a french roll or three big twists.
How often do you shampoo/condition your hair while it is twisted up?
About 1x every 1-3 weeks, depending on the season. I tend to wash more frequently in the summer versus the rest of the year. I tend to wash more frequently if I've been sweating or if my hair is extremely parched.
Wednesday, September 8, 2010
Guest Commentary: Promoting Prevention Through the Affordable Care Act
Rob Simmons, DrPH, MPH, CHES, CPH
Director, Master of Public Health (MPH) Program
Jefferson School of Population Health
It has been nearly six months since the Patient Protection and Affordable Care Act (PPACA) passed Congress and was signed by President Obama. There has been much discussion on the future impact of the new law. Many of the questions raised about the improvement of the health care system and whether it will reduce the skyrocketing increases in healthcare expenses over the past several decades are yet to be answered since significant provisions of the PPACA will not take effect until 2014 or later.
What is clear is that the PPACA will greatly expand health promotion, preventive health services, and the public health infrastructure as a large number of the prevention provisions of the PPACA will begin to take place within the next 6-12 months.
Assistant Secretary of Health Howard Koh, MD, MPH, and Secretary of Health and Human Services Kathleen Sebelius, MPA, provided a perspective on the preventive sections of the PPACA in a recent article in The New England Journal of Medicine. They describe 28 different preventive health sections in the PPACA divided into categories of impact for individuals, businesses and workplaces, communities and states, and the national level.
At the individual level, the most significant provisions are those that provide incentives to participate and pay for risk reduction and for preventive services for those with private health insurance as well as those with both Medicare and Medicaid public health insurance. No longer will there be financial barriers for individuals to obtain evidence-based preventive health screenings, immunizations, risk reduction services such as tobacco cessation, and wellness visits with their health care provider.
For businesses and workplaces, grants will be provided to small businesses to offer comprehensive wellness services. Employers with 15 or more employees will be required to provide reasonable break time and appropriate facilities for nursing mothers to encourage breastfeeding. The Centers for Disease Control will be providing evaluation technical assistance to private industry for their worksite wellness initiatives.
At the community and state government level, grants will be provided to community organizations and state governments to develop, implement, and evaluate evidence-based prevention programs and to provide incentives to promote and maintain healthy behaviors.
At the national level, a wide range of funding is provided to improve and expand health care delivery and patient outcomes, national coordination and leadership, public health infrastructure, the National Health Services Corps., community health centers, private-public partnerships for prevention, diabetes prevention, breast health awareness, oral healthcare preventive activities, and nutrition labeling for restaurant and vending machine menu items.
Since Secretary Sebelius and Assistant Secretary Koh have the primary responsibility for implementation, assessment, and assurance of the PPACA through the development of regulations and subsequent federal actions to support and enforce its provisions, their perspective and priorities are important to note and follow over the next few years. I look forward to reading and, as a public health professional, experiencing, this most significant political effort in the history of our nation to promote health and the use of preventive health services. Whether it will significantly reduce health risks such as obesity and tobacco use and increase protective factors such as breastfeeding and healthy eating, only time will tell. I welcome the ideas of others as outcomes of these initiatives are evaluated and published over the next several years.
To read this article, please click here.
Director, Master of Public Health (MPH) Program
Jefferson School of Population Health
It has been nearly six months since the Patient Protection and Affordable Care Act (PPACA) passed Congress and was signed by President Obama. There has been much discussion on the future impact of the new law. Many of the questions raised about the improvement of the health care system and whether it will reduce the skyrocketing increases in healthcare expenses over the past several decades are yet to be answered since significant provisions of the PPACA will not take effect until 2014 or later.
What is clear is that the PPACA will greatly expand health promotion, preventive health services, and the public health infrastructure as a large number of the prevention provisions of the PPACA will begin to take place within the next 6-12 months.
Assistant Secretary of Health Howard Koh, MD, MPH, and Secretary of Health and Human Services Kathleen Sebelius, MPA, provided a perspective on the preventive sections of the PPACA in a recent article in The New England Journal of Medicine. They describe 28 different preventive health sections in the PPACA divided into categories of impact for individuals, businesses and workplaces, communities and states, and the national level.
At the individual level, the most significant provisions are those that provide incentives to participate and pay for risk reduction and for preventive services for those with private health insurance as well as those with both Medicare and Medicaid public health insurance. No longer will there be financial barriers for individuals to obtain evidence-based preventive health screenings, immunizations, risk reduction services such as tobacco cessation, and wellness visits with their health care provider.
For businesses and workplaces, grants will be provided to small businesses to offer comprehensive wellness services. Employers with 15 or more employees will be required to provide reasonable break time and appropriate facilities for nursing mothers to encourage breastfeeding. The Centers for Disease Control will be providing evaluation technical assistance to private industry for their worksite wellness initiatives.
At the community and state government level, grants will be provided to community organizations and state governments to develop, implement, and evaluate evidence-based prevention programs and to provide incentives to promote and maintain healthy behaviors.
At the national level, a wide range of funding is provided to improve and expand health care delivery and patient outcomes, national coordination and leadership, public health infrastructure, the National Health Services Corps., community health centers, private-public partnerships for prevention, diabetes prevention, breast health awareness, oral healthcare preventive activities, and nutrition labeling for restaurant and vending machine menu items.
Since Secretary Sebelius and Assistant Secretary Koh have the primary responsibility for implementation, assessment, and assurance of the PPACA through the development of regulations and subsequent federal actions to support and enforce its provisions, their perspective and priorities are important to note and follow over the next few years. I look forward to reading and, as a public health professional, experiencing, this most significant political effort in the history of our nation to promote health and the use of preventive health services. Whether it will significantly reduce health risks such as obesity and tobacco use and increase protective factors such as breastfeeding and healthy eating, only time will tell. I welcome the ideas of others as outcomes of these initiatives are evaluated and published over the next several years.
To read this article, please click here.
The China Study II: Cholesterol seems to protect against cardiovascular disease
First of all, many thanks are due to Dr. Campbell and his collaborators for collecting and compiling the data used in this analysis. This data is from this site, created by those researchers to disseminate the data from a study often referred to as the “China Study II”. It has already been analyzed by other bloggers. Notable analyses have been conducted by Ricardo at Canibais e Reis, Stan at Heretic, and Denise at Raw Food SOS.
The analyses in this post differ from those other analyses in various aspects. One of them is that data for males and females were used separately for each county, instead of the totals per county. Only two data points per county were used (for males and females). This increased the sample size of the dataset without artificially reducing variance (for more details, see “Notes” at the end of the post), which is desirable since the dataset is relatively small. This also allowed for the test of commonsense assumptions (e.g., the protective effects of being female), which is always a good idea in a complex analysis because violation of commonsense assumption may suggest data collection or analysis error. On the other hand, it required the inclusion of a sex variable as a control variable in the analysis, which is no big deal.
The analysis was conducted using WarpPLS. Below is the model with the main results of the analysis. (Click on it to enlarge. Use the "CRTL" and "+" keys to zoom in, and CRTL" and "-" to zoom out.) The arrows explore associations between variables, which are shown within ovals. The meaning of each variable is the following: SexM1F2 = sex, with 1 assigned to males and 2 to females; HDLCHOL = HDL cholesterol; TOTCHOL = total cholesterol; MSCHIST = mortality from schistosomiasis infection; and MVASC = mortality from all cardiovascular diseases.
The variables to the left of MVASC are the main predictors of interest in the model – HDLCHOL and TOTCHOL. The ones to the right are control variables – SexM1F2 and MSCHIST. The path coefficients (indicated as beta coefficients) reflect the strength of the relationships. A negative beta means that the relationship is negative; i.e., an increase in a variable is associated with a decrease in the variable that it points to. The P values indicate the statistical significance of the relationship; a P lower than 0.05 generally means a significant relationship (95 percent or higher likelihood that the relationship is “real”).
In summary, this is what the model above is telling us:
- As HDL cholesterol increases, total cholesterol increases significantly (beta=0.48; P<0.01). This is to be expected, as HDL is a main component of total cholesterol, together with VLDL and LDL cholesterol.
- As total cholesterol increases, mortality from all cardiovascular diseases decreases significantly (beta=-0.25; P<0.01). This is to be expected if we assume that total cholesterol is in part an intervening variable between HDL cholesterol and mortality from all cardiovascular diseases. This assumption can be tested through a separate model (more below). Also, there is more to this story, as noted below.
- The effect of HDL cholesterol on mortality from all cardiovascular diseases is insignificant when we control for the effect of total cholesterol (beta=-0.08; P=0.26). This suggests that HDL’s protective role is subsumed by the variable total cholesterol, and also that it is possible that there is something else associated with total cholesterol that makes it protective. Otherwise the effect of total cholesterol might have been insignificant, and the effect of HDL cholesterol significant (the reverse of what we see here).
- Being female is significantly associated with a reduction in mortality from all cardiovascular diseases (beta=-0.16; P=0.01). This is to be expected. In other words, men are women with a few design flaws. (This situation reverses itself a bit after menopause.)
- Mortality from schistosomiasis infection is significantly and inversely associated with mortality from all cardiovascular diseases (beta=-0.28; P<0.01). This is probably due to those dying from schistosomiasis infection not being entered in the dataset as dying from cardiovascular diseases, and vice-versa.
Two other main components of total cholesterol, in addition to HDL cholesterol, are VLDL and LDL cholesterol. These are carried in particles, known as lipoproteins. VLDL cholesterol is usually represented as a fraction of triglycerides in cholesterol equations (e.g., the Friedewald and Iranian equations). It usually correlates inversely with HDL; that is, as HDL cholesterol increases, usually VLDL cholesterol decreases. Given this and the associations discussed above, it seems that LDL cholesterol is a good candidate for the possible “something else associated with total cholesterol that makes it protective”. But waidaminet! Is it possible that the demon particle, the LDL, serves any purpose other than giving us heart attacks?
The graph below shows the shape of the association between total cholesterol (TOTCHOL) and mortality from all cardiovascular diseases (MVASC). The values are provided in standardized format; e.g., 0 is the average, 1 is one standard deviation above the mean, and so on. The curve is the best-fitting S curve obtained by the software (an S curve is a slightly more complex curve than a U curve).
The graph below shows some of the data in unstandardized format, and organized differently. The data is grouped here in ranges of total cholesterol, which are shown on the horizontal axis. The lowest and highest ranges in the dataset are shown, to highlight the magnitude of the apparently protective effect. Here the two variables used to calculate mortality from all cardiovascular diseases (MVASC; see “Notes” at the end of this post) were added. Clearly the lowest mortality from all cardiovascular diseases is in the highest total cholesterol range, 172.5 to 180; and the highest mortality in the lowest total cholesterol range, 120 to 127.5. The difference is quite large; the mortality in the lowest range is approximately 3.3 times higher than in the highest.
The shape of the S-curve graph above suggests that there are other variables that are confounding the results a bit. Mortality from all cardiovascular diseases does seem to generally go down with increases in total cholesterol, but the smooth inflection point at the middle of the S-curve graph suggests a more complex variation pattern that may be influenced by other variables (e.g., smoking, dietary patterns, or even schistosomiasis infection; see “Notes” at the end of this post).
As mentioned before, total cholesterol is strongly influenced by HDL cholesterol, so below is the model with only HDL cholesterol (HDLCHOL) pointing at mortality from all cardiovascular diseases (MVASC), and the control variable sex (SexM1F2).
The graph above confirms the assumption that HDL’s protective role is subsumed by the variable total cholesterol. When the variable total cholesterol is removed from the model, as it was done above, the protective effect of HDL cholesterol becomes significant (beta=-0.27; P<0.01). The control variable sex (SexM1F2) was retained even in this targeted HDL effect model because of the expected confounding effect of sex; females generally tend to have higher HDL cholesterol and less cardiovascular disease than males.
Below, in the “Notes” section (after the “Reference”) are several notes, some of which are quite technical. Providing them separately hopefully has made the discussion above a bit easier to follow. The notes also point at some limitations of the analysis. This data needs to be analyzed from different angles, using multiple models, so that firmer conclusions can be reached. Still, the overall picture that seems to be emerging is at odds with previous beliefs based on the same dataset.
What could be increasing the apparently protective HDL and total cholesterol in this dataset? High consumption of animal foods, particularly foods rich in saturated fat and cholesterol, are strong candidates. Low consumption of vegetable oils rich in linoleic acid, and of foods rich in refined carbohydrates, are also good candidates. Maybe it is a combination of these.
We need more analyses!
Reference:
Kock, N. (2010). WarpPLS 1.0 User Manual. Laredo, Texas: ScriptWarp Systems.
Notes:
- The path coefficients (indicated as beta coefficients) reflect the strength of the relationships; they are a bit like standard univariate (or Pearson) correlation coefficients, except that they take into consideration multivariate relationships (they control for competing effects on each variable).
- The R-squared values reflect the percentage of explained variance for certain variables; the higher they are, the better the model fit with the data. In complex and multi-factorial phenomena such as health-related phenomena, many would consider an R-squared of 0.20 as acceptable. Still, such an R-squared would mean that 80 percent of the variance for a particularly variable is unexplained by the data.
- The P values have been calculated using a nonparametric technique, a form of resampling called jackknifing, which does not require the assumption that the data is normally distributed to be met. This and other related techniques also tend to yield more reliable results for small samples, and samples with outliers (as long as the outliers are “good” data, and are not the result of measurement error).
- Colinearity is an important consideration in models that analyze the effect of multiple predictors on one single variable. This is particularly true for multiple regression models, where there is a temptation of adding many predictors to the model to see which ones come out as the “winners”. This often backfires, as colinearity can severely distort the results. Some multiple regression techniques, such as automated stepwise regression with backward elimination, are particularly vulnerable to this problem. Colinearity is not the same as correlation, and thus is defined and measured differently. Two predictor variables may be significantly correlated and still have low colinearity. A reasonably reliable measure of colinearity is the variance inflation factor. Colinearity was tested in this model, and was found to be low.
- An effort was made here to avoid multiple data points per county (even though this was available for some variables), because this could artificially reduce the variance for each variable, and potentially bias the results. The reason for this is that multiple answers from a single county would normally be somewhat correlated; a higher degree of intra-county correlation than inter-county correlation. The resulting bias would be difficult to control for, via one or more control variables. With only two data points per county, one for males and the other for females, one can control for intra-country correlation by adding a “dummy” sex variable to the analysis, as a control variable. This was done here.
- Mortality from schistosomiasis infection (MSCHIST) is a variable that tends to affect the results in a way that makes it more difficult to make sense of them. Generally this is true for any infectious diseases that significantly affect a population under study. The problem with infection is that people with otherwise good health or habits may get the infection, and people with bad health and habits may not. Since cholesterol is used by the human body to fight disease, it may go up, giving the impression that it is going up for some other reason. Perhaps instead of controlling for its effect, as done here, it would have been better to remove from the analysis those counties with deaths from schistosomiasis infection. (See also this post, and this one.)
- Different parts of the data were collected at different times. It seems that the mortality data is for the period 1986-88, and the rest of the data is for 1989. This may have biased the results somewhat, even though the time lag is not that long, especially if there were changes in certain health trends from one period to the other. For example, major migrations from one county to another could have significantly affected the results.
- The following measures were used, from this online dataset like the other measures. P002 HDLCHOL, for HDLCHOL; P001 TOTCHOL, for TOTCHOL; and M021 SCHISTOc, for MSCHIST.
- SexM1F2 is a “dummy” variable that was coded with 1 assigned to males and 2 to females. As such, it essentially measures the “degree of femaleness” of the respondents. Being female is generally protective against cardiovascular disease, a situation that reverts itself a bit after menopause.
- MVASC is a composite measure of the two following variables, provided as component measures of mortality from all cardiovascular diseases: M058 ALLVASCb (ages 0-34), and M059 ALLVASCc (ages 35-69). A couple of obvious problems: (a) they does not include data on people older than 69; and (b) they seem to capture a lot of diseases, including some that do not seem like typical cardiovascular diseases. A factor analysis was conducted, and the loadings and cross-loadings suggested good validity. Composite reliability was also good. So essentially MVASC is measured here as a “latent variable” with two “indicators”. Why do this? The reason is that it reduces the biasing effects of incomplete data and measurement error (e.g., exclusion of folks older than 69). By the way, there is always some measurement error in any dataset.
- This note is related to measurement error in connection with the indicators for MVASC. There is something odd about the variables M058 ALLVASCb (ages 0-34), and M059 ALLVASCc (ages 35-69). According to the dataset, mortality from cardiovascular diseases for ages 0-34 is typically higher than for 35-69, for many counties. Given the good validity and reliability for MVASC as a latent variable, it is possible that the values for these two indicator variables were simply swapped by mistake.
The analyses in this post differ from those other analyses in various aspects. One of them is that data for males and females were used separately for each county, instead of the totals per county. Only two data points per county were used (for males and females). This increased the sample size of the dataset without artificially reducing variance (for more details, see “Notes” at the end of the post), which is desirable since the dataset is relatively small. This also allowed for the test of commonsense assumptions (e.g., the protective effects of being female), which is always a good idea in a complex analysis because violation of commonsense assumption may suggest data collection or analysis error. On the other hand, it required the inclusion of a sex variable as a control variable in the analysis, which is no big deal.
The analysis was conducted using WarpPLS. Below is the model with the main results of the analysis. (Click on it to enlarge. Use the "CRTL" and "+" keys to zoom in, and CRTL" and "-" to zoom out.) The arrows explore associations between variables, which are shown within ovals. The meaning of each variable is the following: SexM1F2 = sex, with 1 assigned to males and 2 to females; HDLCHOL = HDL cholesterol; TOTCHOL = total cholesterol; MSCHIST = mortality from schistosomiasis infection; and MVASC = mortality from all cardiovascular diseases.
The variables to the left of MVASC are the main predictors of interest in the model – HDLCHOL and TOTCHOL. The ones to the right are control variables – SexM1F2 and MSCHIST. The path coefficients (indicated as beta coefficients) reflect the strength of the relationships. A negative beta means that the relationship is negative; i.e., an increase in a variable is associated with a decrease in the variable that it points to. The P values indicate the statistical significance of the relationship; a P lower than 0.05 generally means a significant relationship (95 percent or higher likelihood that the relationship is “real”).
In summary, this is what the model above is telling us:
- As HDL cholesterol increases, total cholesterol increases significantly (beta=0.48; P<0.01). This is to be expected, as HDL is a main component of total cholesterol, together with VLDL and LDL cholesterol.
- As total cholesterol increases, mortality from all cardiovascular diseases decreases significantly (beta=-0.25; P<0.01). This is to be expected if we assume that total cholesterol is in part an intervening variable between HDL cholesterol and mortality from all cardiovascular diseases. This assumption can be tested through a separate model (more below). Also, there is more to this story, as noted below.
- The effect of HDL cholesterol on mortality from all cardiovascular diseases is insignificant when we control for the effect of total cholesterol (beta=-0.08; P=0.26). This suggests that HDL’s protective role is subsumed by the variable total cholesterol, and also that it is possible that there is something else associated with total cholesterol that makes it protective. Otherwise the effect of total cholesterol might have been insignificant, and the effect of HDL cholesterol significant (the reverse of what we see here).
- Being female is significantly associated with a reduction in mortality from all cardiovascular diseases (beta=-0.16; P=0.01). This is to be expected. In other words, men are women with a few design flaws. (This situation reverses itself a bit after menopause.)
- Mortality from schistosomiasis infection is significantly and inversely associated with mortality from all cardiovascular diseases (beta=-0.28; P<0.01). This is probably due to those dying from schistosomiasis infection not being entered in the dataset as dying from cardiovascular diseases, and vice-versa.
Two other main components of total cholesterol, in addition to HDL cholesterol, are VLDL and LDL cholesterol. These are carried in particles, known as lipoproteins. VLDL cholesterol is usually represented as a fraction of triglycerides in cholesterol equations (e.g., the Friedewald and Iranian equations). It usually correlates inversely with HDL; that is, as HDL cholesterol increases, usually VLDL cholesterol decreases. Given this and the associations discussed above, it seems that LDL cholesterol is a good candidate for the possible “something else associated with total cholesterol that makes it protective”. But waidaminet! Is it possible that the demon particle, the LDL, serves any purpose other than giving us heart attacks?
The graph below shows the shape of the association between total cholesterol (TOTCHOL) and mortality from all cardiovascular diseases (MVASC). The values are provided in standardized format; e.g., 0 is the average, 1 is one standard deviation above the mean, and so on. The curve is the best-fitting S curve obtained by the software (an S curve is a slightly more complex curve than a U curve).
The graph below shows some of the data in unstandardized format, and organized differently. The data is grouped here in ranges of total cholesterol, which are shown on the horizontal axis. The lowest and highest ranges in the dataset are shown, to highlight the magnitude of the apparently protective effect. Here the two variables used to calculate mortality from all cardiovascular diseases (MVASC; see “Notes” at the end of this post) were added. Clearly the lowest mortality from all cardiovascular diseases is in the highest total cholesterol range, 172.5 to 180; and the highest mortality in the lowest total cholesterol range, 120 to 127.5. The difference is quite large; the mortality in the lowest range is approximately 3.3 times higher than in the highest.
The shape of the S-curve graph above suggests that there are other variables that are confounding the results a bit. Mortality from all cardiovascular diseases does seem to generally go down with increases in total cholesterol, but the smooth inflection point at the middle of the S-curve graph suggests a more complex variation pattern that may be influenced by other variables (e.g., smoking, dietary patterns, or even schistosomiasis infection; see “Notes” at the end of this post).
As mentioned before, total cholesterol is strongly influenced by HDL cholesterol, so below is the model with only HDL cholesterol (HDLCHOL) pointing at mortality from all cardiovascular diseases (MVASC), and the control variable sex (SexM1F2).
The graph above confirms the assumption that HDL’s protective role is subsumed by the variable total cholesterol. When the variable total cholesterol is removed from the model, as it was done above, the protective effect of HDL cholesterol becomes significant (beta=-0.27; P<0.01). The control variable sex (SexM1F2) was retained even in this targeted HDL effect model because of the expected confounding effect of sex; females generally tend to have higher HDL cholesterol and less cardiovascular disease than males.
Below, in the “Notes” section (after the “Reference”) are several notes, some of which are quite technical. Providing them separately hopefully has made the discussion above a bit easier to follow. The notes also point at some limitations of the analysis. This data needs to be analyzed from different angles, using multiple models, so that firmer conclusions can be reached. Still, the overall picture that seems to be emerging is at odds with previous beliefs based on the same dataset.
What could be increasing the apparently protective HDL and total cholesterol in this dataset? High consumption of animal foods, particularly foods rich in saturated fat and cholesterol, are strong candidates. Low consumption of vegetable oils rich in linoleic acid, and of foods rich in refined carbohydrates, are also good candidates. Maybe it is a combination of these.
We need more analyses!
Reference:
Kock, N. (2010). WarpPLS 1.0 User Manual. Laredo, Texas: ScriptWarp Systems.
Notes:
- The path coefficients (indicated as beta coefficients) reflect the strength of the relationships; they are a bit like standard univariate (or Pearson) correlation coefficients, except that they take into consideration multivariate relationships (they control for competing effects on each variable).
- The R-squared values reflect the percentage of explained variance for certain variables; the higher they are, the better the model fit with the data. In complex and multi-factorial phenomena such as health-related phenomena, many would consider an R-squared of 0.20 as acceptable. Still, such an R-squared would mean that 80 percent of the variance for a particularly variable is unexplained by the data.
- The P values have been calculated using a nonparametric technique, a form of resampling called jackknifing, which does not require the assumption that the data is normally distributed to be met. This and other related techniques also tend to yield more reliable results for small samples, and samples with outliers (as long as the outliers are “good” data, and are not the result of measurement error).
- Colinearity is an important consideration in models that analyze the effect of multiple predictors on one single variable. This is particularly true for multiple regression models, where there is a temptation of adding many predictors to the model to see which ones come out as the “winners”. This often backfires, as colinearity can severely distort the results. Some multiple regression techniques, such as automated stepwise regression with backward elimination, are particularly vulnerable to this problem. Colinearity is not the same as correlation, and thus is defined and measured differently. Two predictor variables may be significantly correlated and still have low colinearity. A reasonably reliable measure of colinearity is the variance inflation factor. Colinearity was tested in this model, and was found to be low.
- An effort was made here to avoid multiple data points per county (even though this was available for some variables), because this could artificially reduce the variance for each variable, and potentially bias the results. The reason for this is that multiple answers from a single county would normally be somewhat correlated; a higher degree of intra-county correlation than inter-county correlation. The resulting bias would be difficult to control for, via one or more control variables. With only two data points per county, one for males and the other for females, one can control for intra-country correlation by adding a “dummy” sex variable to the analysis, as a control variable. This was done here.
- Mortality from schistosomiasis infection (MSCHIST) is a variable that tends to affect the results in a way that makes it more difficult to make sense of them. Generally this is true for any infectious diseases that significantly affect a population under study. The problem with infection is that people with otherwise good health or habits may get the infection, and people with bad health and habits may not. Since cholesterol is used by the human body to fight disease, it may go up, giving the impression that it is going up for some other reason. Perhaps instead of controlling for its effect, as done here, it would have been better to remove from the analysis those counties with deaths from schistosomiasis infection. (See also this post, and this one.)
- Different parts of the data were collected at different times. It seems that the mortality data is for the period 1986-88, and the rest of the data is for 1989. This may have biased the results somewhat, even though the time lag is not that long, especially if there were changes in certain health trends from one period to the other. For example, major migrations from one county to another could have significantly affected the results.
- The following measures were used, from this online dataset like the other measures. P002 HDLCHOL, for HDLCHOL; P001 TOTCHOL, for TOTCHOL; and M021 SCHISTOc, for MSCHIST.
- SexM1F2 is a “dummy” variable that was coded with 1 assigned to males and 2 to females. As such, it essentially measures the “degree of femaleness” of the respondents. Being female is generally protective against cardiovascular disease, a situation that reverts itself a bit after menopause.
- MVASC is a composite measure of the two following variables, provided as component measures of mortality from all cardiovascular diseases: M058 ALLVASCb (ages 0-34), and M059 ALLVASCc (ages 35-69). A couple of obvious problems: (a) they does not include data on people older than 69; and (b) they seem to capture a lot of diseases, including some that do not seem like typical cardiovascular diseases. A factor analysis was conducted, and the loadings and cross-loadings suggested good validity. Composite reliability was also good. So essentially MVASC is measured here as a “latent variable” with two “indicators”. Why do this? The reason is that it reduces the biasing effects of incomplete data and measurement error (e.g., exclusion of folks older than 69). By the way, there is always some measurement error in any dataset.
- This note is related to measurement error in connection with the indicators for MVASC. There is something odd about the variables M058 ALLVASCb (ages 0-34), and M059 ALLVASCc (ages 35-69). According to the dataset, mortality from cardiovascular diseases for ages 0-34 is typically higher than for 35-69, for many counties. Given the good validity and reliability for MVASC as a latent variable, it is possible that the values for these two indicator variables were simply swapped by mistake.
Monday, September 6, 2010
Low omega-6 to omega-3 ratio: Grain-fed meats or industrial vegetable oils?
Just a little note on the use of language. Clearly there is no such a thing as grain-fed or grass-fed beef, because one does not feed beef anything. One feeds cattle grain or grass, and then the resulting beef is said to be “grain-fed” or “grass-fed”. It is a manner of speaking that facilitates discourse, which is why it is used here.
To compensate for this digression, let me show you a graph, which pretty much summarizes the "punch line" of this post. The graph below shows the omega-6 fat contents of 1 lb (454 g) of grain-fed beef and 1 tablespoon (roughly 14 g) of a typical industrial vegetable oil (safflower oil). As you can see, there is a lot more omega-6 in the much smaller amount of industrial vegetable oil. A gram-for-gram comparison would practically make the beef content bar disappear.
It has been estimated that our Paleolithic ancestors consumed a diet with an omega-6 to omega-3 ratio of about 1. While other estimates exist, the general consensus seems to be that that ratio was not much greater than 5. Western diets, in contrast, typically have omega-6 to omega-3 ratios of between 15 and 40. In some cases, the ratio is even higher.
Omega-6 fats are essential fats, meaning that they must be part of one’s diet. Fats make up about 60 percent of our brain. About 20 percent is made up of omega-6 and omega-3 fats. The primary omega-6 fat found in our brain is arachidonic acid, which is either synthesized by our body based on linoleic acid from plant foods or obtained directly from animal foods such as meat and eggs. The predominant omega-3 fat found in our brain is docosahexaenoic acid (DHA), of which certain types of fish and algae are rich sources.
Inflammation is an important process in the human body, without which wounds would never heal. Incidentally, muscle gain would not occur without inflammation either. Strength training causes muscle damage and inflammation, after which recovery leads to muscle gain. Omega-6 fats play an important role in inflammation. Generally, they are pro-inflammatory.
Too much inflammation, particularly in a chronic fashion, is believed to be very detrimental to our health. A very high omega-6 to omega-3 ratio seems to cause excessive and chronic inflammation. The reason is that omega-3 fats are generally anti-inflammatory, counteracting the pro-inflammatory action of omega-6 fats. Over time, a very high omega-6 to omega-3 ratio is believed to cause a number of Western diseases. Among them are cardiovascular complications, cancer, and various autoimmune diseases.
So, should you worry about too much omega-6 from grain-fed meats?
If you think that the answer is “yes”, consider this. Apparently the (arguably) longest-living group in the world, the non-Westernized Okinawans, consume plenty of pork. Pork is a staple of their traditional diet. It is true that the average cut will have an omega-6 to omega-3 ratio of more than 7, which is not very favorable. Pork in general, whether grain-fed or not, is relatively high in omega-6 fats. As a side note, pork is not a good source of linoleic acid (found in plants), even though it is a rich source of arachidonic acid, the omega-6 fat synthesized from linoleic acid by various animals.
It is difficult to estimate the exact amounts of omega-6 and omega-3 fats from grain-fed cuts of meat; different sources provide different estimates. Here are some reasonable estimates based on various sources, including Nutritiondata.com. A typical 100 g portion of grain-fed pork should contain about 690 mg of omega-6 fats, and 120 mg of omega-3 fats. A typical 100 g portion of grain-fed beef should have about 234 mg of omega-6 fats, and 12 mg of omega-3 fats. It does not take that much omega-3 to counterbalance the omega-6 obtained from grain-fed pork or beef, even if one eats a lot of them. Two softgels of fish oil will normally contain about 720 mg of omega-3 fats (they will also come with 280 mg of omega-6 fats). Three sardines will have over 2 g of omega-3 fats, and less than 200 mg of omega-6 fats.
Industrial vegetable oils (made from, e.g., safflower seeds, soybean, and sunflower seeds) are very, very rich sources of omega-6 fats, in the form of linoleic acid. There is a lot more omega-6 in them than in grain-fed meats. One tablespoon of safflower oil contains over 10 g of omega-6 fats, in the form of linoleic acid, and virtually zero omega-3 fats. About 2 kg (4.4 lbs) of grain-fed pork, and 5 kg (11 lbs) of grain-fed beef will give you that much omega-6; but they will also come with omega-3.
How much fish oil does one need to neutralize 10 g of pure omega-6 fats? A lot! And there is a problem. Excessive fish oil consumption may be toxic to the liver.
If you cook with industrial vegetable oils rich in linoleic acid (this excludes olive and coconut oils), or eat out a lot in restaurants that use them (the vast majority), you will probably be consuming significantly more than 10 g of omega-6 fats per day. The likely negative health effects of eating grain-fed meats pales in comparison with the likely negative health effects of this much omega-6 fats from industrial vegetable oils.
You should reduce as much as possible your consumption of industrial vegetable oils rich in linoleic acid, as well as other products that use them (e.g., margarine). Keep in mind that industrial vegetable oils are in many, many industrialized foods; even canned sardines, if they are canned with soybean oil.
It is also advisable to couple this with moderate consumption of fish rich in omega-3, such as sardines and salmon. (See this post for a sardine recipe.) Taking large doses of fish oil every day may not be such a good idea.
Should you also consume only grass-fed meat? Do it if you can. But, if you cannot, maybe you shouldn’t worry too much about it. This also applies to eggs, dairy, and other animal products.
References:
Elliott, W.H., & Elliott, D.C. (2009). Biochemistry and molecular biology. New York: NY: Oxford University Press.
Ramsden, C.E., Faurot, K.R., Carrera-Bastos, P., Cordain, L., De Lorgeril, M., & Sperling (2009). Dietary fat quality and coronary heart disease prevention: A unified theory based on evolutionary, historical, global, and modern perspectives. Current Treatment Options in Cardiovascular Medicine, 11(4), 289-301.
Schmidt, M.A. (1997). Smart fats: How dietary fats and oils affect mental, physical and emotional intelligence. Berkeley, CA: North Atlantic Books.
To compensate for this digression, let me show you a graph, which pretty much summarizes the "punch line" of this post. The graph below shows the omega-6 fat contents of 1 lb (454 g) of grain-fed beef and 1 tablespoon (roughly 14 g) of a typical industrial vegetable oil (safflower oil). As you can see, there is a lot more omega-6 in the much smaller amount of industrial vegetable oil. A gram-for-gram comparison would practically make the beef content bar disappear.
It has been estimated that our Paleolithic ancestors consumed a diet with an omega-6 to omega-3 ratio of about 1. While other estimates exist, the general consensus seems to be that that ratio was not much greater than 5. Western diets, in contrast, typically have omega-6 to omega-3 ratios of between 15 and 40. In some cases, the ratio is even higher.
Omega-6 fats are essential fats, meaning that they must be part of one’s diet. Fats make up about 60 percent of our brain. About 20 percent is made up of omega-6 and omega-3 fats. The primary omega-6 fat found in our brain is arachidonic acid, which is either synthesized by our body based on linoleic acid from plant foods or obtained directly from animal foods such as meat and eggs. The predominant omega-3 fat found in our brain is docosahexaenoic acid (DHA), of which certain types of fish and algae are rich sources.
Inflammation is an important process in the human body, without which wounds would never heal. Incidentally, muscle gain would not occur without inflammation either. Strength training causes muscle damage and inflammation, after which recovery leads to muscle gain. Omega-6 fats play an important role in inflammation. Generally, they are pro-inflammatory.
Too much inflammation, particularly in a chronic fashion, is believed to be very detrimental to our health. A very high omega-6 to omega-3 ratio seems to cause excessive and chronic inflammation. The reason is that omega-3 fats are generally anti-inflammatory, counteracting the pro-inflammatory action of omega-6 fats. Over time, a very high omega-6 to omega-3 ratio is believed to cause a number of Western diseases. Among them are cardiovascular complications, cancer, and various autoimmune diseases.
So, should you worry about too much omega-6 from grain-fed meats?
If you think that the answer is “yes”, consider this. Apparently the (arguably) longest-living group in the world, the non-Westernized Okinawans, consume plenty of pork. Pork is a staple of their traditional diet. It is true that the average cut will have an omega-6 to omega-3 ratio of more than 7, which is not very favorable. Pork in general, whether grain-fed or not, is relatively high in omega-6 fats. As a side note, pork is not a good source of linoleic acid (found in plants), even though it is a rich source of arachidonic acid, the omega-6 fat synthesized from linoleic acid by various animals.
It is difficult to estimate the exact amounts of omega-6 and omega-3 fats from grain-fed cuts of meat; different sources provide different estimates. Here are some reasonable estimates based on various sources, including Nutritiondata.com. A typical 100 g portion of grain-fed pork should contain about 690 mg of omega-6 fats, and 120 mg of omega-3 fats. A typical 100 g portion of grain-fed beef should have about 234 mg of omega-6 fats, and 12 mg of omega-3 fats. It does not take that much omega-3 to counterbalance the omega-6 obtained from grain-fed pork or beef, even if one eats a lot of them. Two softgels of fish oil will normally contain about 720 mg of omega-3 fats (they will also come with 280 mg of omega-6 fats). Three sardines will have over 2 g of omega-3 fats, and less than 200 mg of omega-6 fats.
Industrial vegetable oils (made from, e.g., safflower seeds, soybean, and sunflower seeds) are very, very rich sources of omega-6 fats, in the form of linoleic acid. There is a lot more omega-6 in them than in grain-fed meats. One tablespoon of safflower oil contains over 10 g of omega-6 fats, in the form of linoleic acid, and virtually zero omega-3 fats. About 2 kg (4.4 lbs) of grain-fed pork, and 5 kg (11 lbs) of grain-fed beef will give you that much omega-6; but they will also come with omega-3.
How much fish oil does one need to neutralize 10 g of pure omega-6 fats? A lot! And there is a problem. Excessive fish oil consumption may be toxic to the liver.
If you cook with industrial vegetable oils rich in linoleic acid (this excludes olive and coconut oils), or eat out a lot in restaurants that use them (the vast majority), you will probably be consuming significantly more than 10 g of omega-6 fats per day. The likely negative health effects of eating grain-fed meats pales in comparison with the likely negative health effects of this much omega-6 fats from industrial vegetable oils.
You should reduce as much as possible your consumption of industrial vegetable oils rich in linoleic acid, as well as other products that use them (e.g., margarine). Keep in mind that industrial vegetable oils are in many, many industrialized foods; even canned sardines, if they are canned with soybean oil.
It is also advisable to couple this with moderate consumption of fish rich in omega-3, such as sardines and salmon. (See this post for a sardine recipe.) Taking large doses of fish oil every day may not be such a good idea.
Should you also consume only grass-fed meat? Do it if you can. But, if you cannot, maybe you shouldn’t worry too much about it. This also applies to eggs, dairy, and other animal products.
References:
Elliott, W.H., & Elliott, D.C. (2009). Biochemistry and molecular biology. New York: NY: Oxford University Press.
Ramsden, C.E., Faurot, K.R., Carrera-Bastos, P., Cordain, L., De Lorgeril, M., & Sperling (2009). Dietary fat quality and coronary heart disease prevention: A unified theory based on evolutionary, historical, global, and modern perspectives. Current Treatment Options in Cardiovascular Medicine, 11(4), 289-301.
Schmidt, M.A. (1997). Smart fats: How dietary fats and oils affect mental, physical and emotional intelligence. Berkeley, CA: North Atlantic Books.
Subscribe to:
Posts (Atom)